Translate this page into:
Transjugular Intrahepatic Portosystemic Shunt Creation in Situs Inversus Totalis - A Case Report

Corresponding Author: Nischal G Kundaragi, Department of Interventional Radiology and Interventional Oncology, Aster CMI Hospital, New Airport Road, Bengaluru, Karnataka, 560092, India. E-mail: drngkradiology@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kundaragi NG, Ganjoo N. Transjugular Intrahepatic Portosystemic Shunt Creation in Situs Inversus Totalis - A Case Report. Am J Interv Radiol 2018, 2(11) 1-3.
Abstract
We describe the third case of successful transjugular intrahepatic portosystemic shunt creation for the treatment of refractory ascites due to cirrhosis in a known case of situs inversus totalis.
Keywords
Cirrhosis
Situs inversus totalis
Transjugular intrahepatic portosystemic shunt
INTRODUCTION
Situs inversus totalis is a rare congenital condition in which there is total transposition of abdominal and thoracic viscera in the sagittal plane. Situs inversus occurs in about 1 in 10,000–20,000 live births.[1] Etiology of situs inversus is still unknown. However, it has been proposed to have autosomal recessive inheritance.[2] It is often detected incidentally by radiological investigations. In fact, there is little information about the abdominal manifestations of situs anomalies in adults.[3] Association of cirrhosis with refractory ascites and situs inversus totalis in an adult patient is rare and purely incidental. Transjugular intrahepatic portosystemic shunt (TIPS) is an established procedure to treat complications of portal hypertension. Two cases of TIPS creation in situs inversus have been reported in 2002.[4,5] We briefly report another rare case of successful TIPS creation in a cirrhotic patient with refractory ascites.
CASE REPORT
A 53-year-old male patient, known case of situs inversus totalis and cryptogenic cirrhosis, presented with refractory ascites. The patient was diabetic for 10 years. Serum creatinine was 1.5 mg/dL, total bilirubin was 1.64 mg/dL, serum sodium was 142 meq/L, serum albumin was 3.7 g/dL, platelet count was 68 k/micL, and INR was 1.2. Model for end-stage liver disease (MELD) score was 14. No hepatic encephalopathy was observed.
Pre-procedure, contrast-enhanced computed tomography (CT) scan was performed to evaluate the vascular anatomy. Contrast-enhanced CT scan coronal image showing liver and portal vein (PV) on the left side, spleen and stomach on the right side and dextrocardia (Figure 1a).
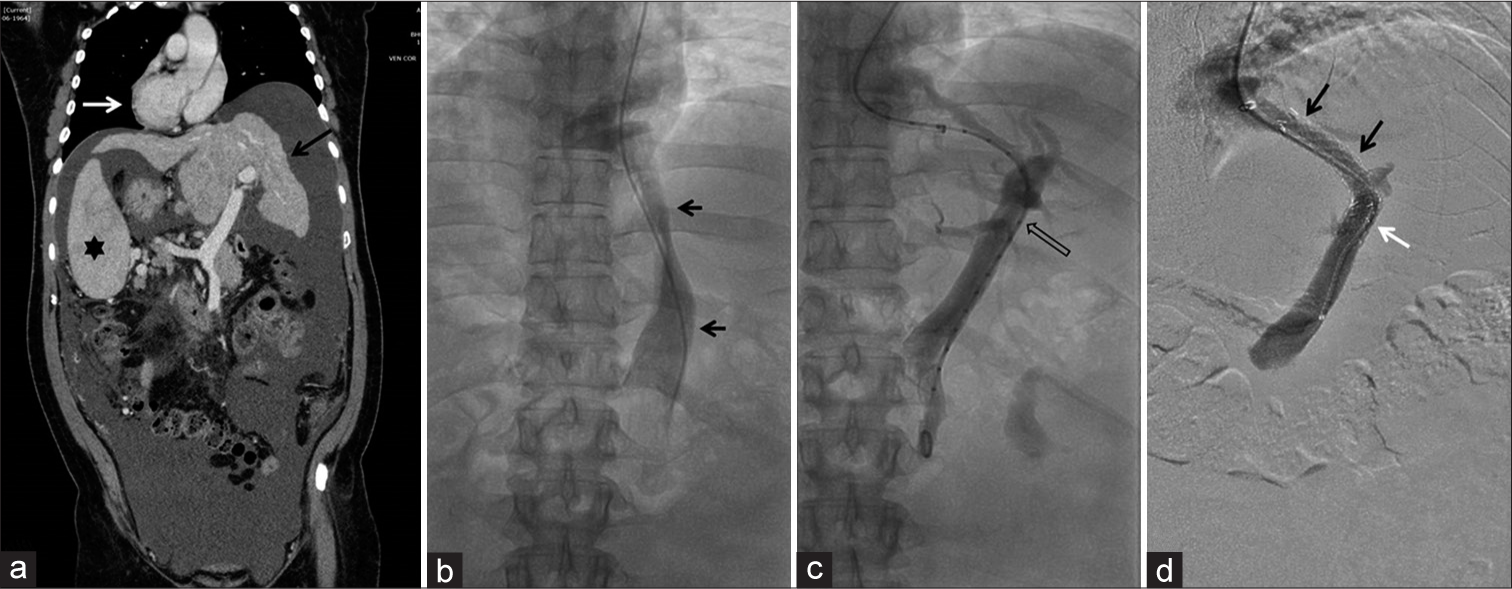
- A 53-year-old male, known case of cirrhosis, presented with refractory ascites. (a) Contrast-enhanced computed tomography scan coronal image shows liver on the left side (black arrow), spleen on the right side (asterisk) and dextrocardia (white arrow). (b) Digital venogram showing inferior vena cava on the left side of midline (black arrows). (c) Pre-stenting, digital portal venogram showing main portal vein (PV) (black open arrow) and its branches. (d) Post-stenting, digital venogram showing stent with uncovered (white arrow) and covered portions (black arrows) with opacified proximal intrahepatic PV branches (black arrowhead).
TIPS procedure was performed through the left transjugular and the left superior vena cava (LSVC) approach. Inferior vena cava (IVC) was seen on the left side of spine (Figure 1b). The left hepatic vein (morphological right hepatic vein) was cannulated and hepatic venous pressure measurements were done. Rösch-Uchida set (Cook Medical, Bloomington, IN) was used for puncture. The left main PV was punctured from the left hepatic vein (morphological right hepatic vein to the right main PV). Ultrasound guidance was used for puncture. Puncture was an exact mirror image of the usual technique with puncture needle turned and directed anteromedial and right of the patient (normally turned anteromedial and left of the patient). Serial balloon dilatation of the tract was performed. Pre-stenting, portal venogram was performed (Figure 1c). A self-expandable Niti-S (Taewoong, Seoul, Korea) TIPS stent of size 10 mm × 90 mm (70 mm covered intrahepatic portion and 20 mm uncovered PV portion) was deployed. Post-stenting, 10 mm balloon dilatation was done. Digital subtraction portal venogram revealed widely patent portosystemic shunt between the left PV and left hepatic vein (i.e. morphologic right PV and right hepatic vein, Figure 1d). Post-stenting, pressure gradient was reduced from 20 mmHg to 9 mmHg. Anticoagulation was used similar to routine TIPS cases. Spectral Doppler ultrasound done post-procedure and on the next day showed normal velocity (average 130 cm/s) in portosystemic shunt. The patient is doing well for 6 months, no recurrence of ascites or hepatic encephalopathy was observed. Currently, he is awaiting deceased donor liver transplant.
DISCUSSION
TIPS is one of the valid therapeutic procedures for the treatment of portal hypertension and its complications. Indications for TIPS include acute variceal hemorrhage, refractory ascites, hepatic hydrothorax, hepatorenal syndrome, Budd–Chiari syndrome, hepatopulmonary syndrome, and PV thrombosis. The guidelines to perform this procedure have already been established on the basis of the normal vascular anatomy and different interventional radiological techniques. TIPS creation in abnormal anatomy is always challenging.
Association of situs inversus totalis in a patient with liver cirrhosis and refractory ascites is very rare.
The standard access for TIPS procedure is the right internal jugular vein approach, although some authors have reported the left internal jugular vein approach when the right side approach is not possible because of internal jugular vein thrombosis or stenosis.[6]
Different techniques have been described to correctly visualize the portal venous system in difficult anatomy, such as placing an angiographic catheter, small wire, or retrieval basket within the PV; placing a catheter into the left PV through a patent paraumbilical vein; marking the hepatic artery with a microcatheter; performing the procedure with the assistance of ultrasound, magnetic resonance imaging, indirect contrast portography, wedge CO2 portography; and using intravascular ultrasound to localize the PV.[7] So far, only a few cases of successful TIPS placement in aberrant anatomy through LSVC approach have been reported.[4,5,8,9] We used the left jugular vein and LSVC approach and ultrasound guidance to access the portal venous system.
Two cases of TIPS creation in situs inversus totalis have been reported till date.[4,5] In one case, TIPS was created between morphological right hepatic vein and right PV and the patient did well at 3-month follow-up with patent stent. In another case, TIPS was created between middle hepatic vein and morphological right PV and the patient died at 1-month follow-up, due to heart failure with a patent shunt. Two overlapping stents were used in both the previous cases; however, we used a single long stent.
Rarity of case with mirror image of vascular anatomy and organs makes TIPS creation challenging in situs inversus totalis. Interventional radiologists should be aware of this rare congenital anomaly, vascular anatomy, and technical modifications used to perform successful TIPS procedure.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Situs inversus totalis; a statistical review of data on 76 cases with special reference to disease of the biliary tract. Arch Surg. 1949;58:724-30.
- [CrossRef] [Google Scholar]
- Laparoscopic cholecystectomy and appendectomy in situs inversus totalis. JSLS. 2000;4:251-4.
- [Google Scholar]
- Abdominal manifestations of situs anomalies in adults. Radiographics. 2002;22:1439-56.
- [CrossRef] [PubMed] [Google Scholar]
- Transjugular intrahepatic portosystemic shunt creation in a patient with situs inversus. J Vasc Interv Radiol. 2002;13:755-6.
- [CrossRef] [Google Scholar]
- TIPS creation in a patient with situs inversus totalis. Cardiovasc Intervent Radiol. 2002;25:447-9.
- [CrossRef] [PubMed] [Google Scholar]
- Use of the left internal jugular vein approach for transjugular portosystemic shunt. AJR Am J Roentgenol. 1998;171:1637-9.
- [CrossRef] [PubMed] [Google Scholar]
- The difficult transjugular intrahepatic portosystemic shunt: Alternative techniques and “tips” to successful shunt creation. Semin Intervent Radiol. 2005;22:300-8.
- [CrossRef] [PubMed] [Google Scholar]
- Transjugular intrahepatic portosystemic shunt with accidental diagnosis of persistence of the left superior vena cava. World J Gastroenterol. 2010;16:1158-60.
- [CrossRef] [PubMed] [Google Scholar]
- Transjugular intrahepatic portosystemic shunt placement in a patient with absent right superior vena cava and persistent left superior vena cava. AJR Am J Roentgenol. 1999;173:631-2.
- [CrossRef] [PubMed] [Google Scholar]






