Translate this page into:
Mechanical thrombectomy with the novel InThrill thrombectomy catheter for portal vein thrombosis and occluded transjugular intrahepatic portosystemic shunt: A case series

*Corresponding author: Jennifer Laporte, Division of Interventional Radiology, Brevard Physician Associates, Melbourne, Florida, United States. jlaportecaballero@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Laporte J, Mittleider D. Mechanical thrombectomy with the novel InThrill thrombectomy catheter for portal vein thrombosis and occluded transjugular intrahepatic portosystemic shunt: A case series. Am J Interv Radiol. 2024;8:3. doi: 10.25259/AJIR_49_2023
Abstract
Portal vein thrombosis (PVT) is commonly treated with anticoagulation alone, though rates of recanalization with anticoagulation vary widely. Four patients with PVT (n = 3) or occluded transjugular intrahepatic portosystemic shunt (n = 1) were treated using the InThrill thrombectomy catheter. Mechanical thrombectomy was technically successful in all patients, resulting in >90% thrombus removal from each patient. Three patients were discharged home, and patency and symptom resolution were maintained at a 2-month follow-up. One patient was discharged to rehabilitation due to comorbidities and expired after presenting with a myocardial infarction and pneumonia 2 weeks post-procedure.
Keywords
Mechanical thrombectomy
Portal vein thrombosis
Transjugular intrahepatic portosystemic shunt
INTRODUCTION
Portal vein thrombosis (PVT) is commonly treated with anticoagulation alone, though recanalization rates with anticoagulation varies widely from 40% to 77%.[1,2] Failure to treat symptomatic PVT can result in complications associated with portal hypertension, hepatic decompensation, mesenteric ischemia, and chronic cavernous transformation.[1]
Here, we present the novel application of the InThrill thrombectomy catheter (Inari Medical, Irvine, CA, USA) to treat PVT or an occluded transjugular intrahepatic portosystemic shunt (TIPS). The 8-French thrombectomy catheter is designed to remove acute to chronic thrombus in 4–10 mm diameter vessels through mechanical thrombectomy with its self-expanding nitinol coring element that can expand up to 18 mm in diameter, allowing for wall apposition and engagement of wall-adherent thrombus in the mesenteric system. The InThrill Thrombectomy System is indicated for the non-surgical removal of thrombi and emboli from blood vessels in the peripheral vasculature, including synthetic grafts. This thrombectomy catheter has demonstrated efficient removal of acute to chronic appearing thrombus in a variety of small diameter peripheral veins; including the treatment of upper extremity thrombosis and thrombosed hemodialysis accesses.[3-5] These initial reports, coupled with the catheter’s small profile, prompted the use of the device to treat PVT and occluded transjugular intrahepatic portosystemic shunt (TIPS).
CASE REPORTS
Four consecutive patients with symptomatic PVT (n = 3) or occluded TIPS (n = 1) were treated with mechanical thrombectomy and retrospectively reviewed [Table 1]. Pre-procedure laboratory results and model for end-stage liver disease (MELD) scores are shown in Table 2. Internal jugular (IJ) vein access was achieved through the micropuncture needle with ultrasound guidance. For 3 patients, a Viatorr TIPS endoprosthesis (Gore Medical, Flagstaff, AZ, USA) was placed under general anesthesia through a TIPS access needle passed from the right hepatic vein into a PV branch under fluoroscopic, intravascular ultrasound (IVUS), and intracardiac echocardiography guidance. Balloon dilation of the TIPS endoprosthesis was performed. Thrombectomy was performed over the-wire using an InThrill thrombectomy catheter with a 16-French Introducer sheath (Cook Medical, Bloomington, IN, USA) used to hold access and a 13-French ClotTriever sheath (Inari Medical, Irvine, CA, USA). InThrill was advanced into the TIPS, portal vein (PV), and if necessary, the superior mesenteric veins (SMV). Four passes with the InThrill thrombectomy catheter were performed in each case, with aspiration through the ClotTriever sheath after each pass, to yield >90% thrombus removal from each patient. Estimated blood loss was <50 mL for each patient. Patency was confirmed with venography [Figure 1].
| Case # | Age/sex | Past medical history | Presentation | Diagnosis | Prior treatment (s) | Procedures performed | Outcome |
|---|---|---|---|---|---|---|---|
| 1 | 71 Male | • Beta-thalassemia • Hypertension • Hyperlipidemia |
• -Acute burning upper abdominal pain, fullness, nausea, vomiting, and constipation | • Thrombosis of PV, SMV, and distal branches with associated mesenteric edema | • Heparin drip | • TIPS placed • - Thrombectomy of PV and SMV |
• Significant reduction in thrombus volume and restored outflow from SMV • Patency maintained at 2-month follow-up |
| 2 | 67 Male | • Non-alcoholic steatohepatitis with portal hypertension • CHF • COPD • Type 2 diabetes • Thrombocytopenia -Sleep apnea • Chronic back pain • GI bleed |
• Elevated pro-BNP and abnormal chest radiograph with findings concerning for multifocal pneumonia versus pulmonary edema | • Thrombosis of PV, large esophageal varices, erosive esophagitis, severe portal hypertensive gastropathy | • Apixaban | • TIPS placed • Thrombectomy of PV |
Significant amount of chronic thrombus removed from PV Patient expired 2-week post-procedure due to comorbidities |
| 3 | 62 Female | • Alcohol-related chronic liver disease -Portal hypertension • Bleeding esophageal varices • Gastric antral vascular ectasia • Recurrent GI bleed -Hypertension • Chronic gastritis |
• Abdominal pain and shortness of breath for 3 days | • -Occluded TIPS with abdominal ascites, right pleural effusion | • -TIPS • -Argon plasma coagulation 48 h before InThrill |
• Thrombectomy of preexisting TIPS • - Angioplasty of TIPS |
• Widely patent TIPS with restored hepatopetal flow • - Patency maintained at 2-month follow-up |
| 4 | 25 Female | • -No significant medical history • -Started oral contraceptives pills 2 months prior |
• Severe abdominal pain for 6 days | • Thrombosis of PV, SMV, and distal branches with mesenteric edema | • Heparin drip | • TIPS placement • Thrombectomy of PV, SMV, and distal branches • Stent placed in SMV • Angioplasty of SMV |
• Significant amount of acute and chronic thrombus removed • No significant residual stenosis • Patency maintained at 2-month follow-up |
PV: Portal vein, SMV: Superior mesenteric vein, CHF: Congestive heart failure, COPD: Chronic obstructive pulmonary disease, GI: Gastrointestinal, TIPS: Transjugular intrahepatic portosystemic shunt
| Case 1 | Case 2 | Case 3 | Case 4 | |
|---|---|---|---|---|
| WBC (thou/cumm) | 12.49 | 15.35 | 8.8 | 6.32 |
| Hemoglobin (g/dL) | 12.9 | 6.6 | 10 | 9.5 |
| Platelets (thou/cumm) | 105 | 38 | 242 | 213 |
| INR | 1.08 | 1.42 | 1.46 | 1.25 |
| Total bilirubin (mg/dL) | 0.76 | 1.62 | 1.34 | 0.28 |
| ALT (U/L) | 145 | 27 | 17 | 21 |
| AST (U/L) | 66 | 32 | 31 | 45 |
| Lactic acid (mmol/L) | 2.4 | NR | 1.4 | 1 |
| MELD score | NA | 11 | 17 | NA |
WBC: White blood cell count, INR: International normalized ratio, ALT: Alanine transaminase, AST: Aspartate transaminase, MELD: Model for end-stage liver disease, U/L: Units/Liter, NA: Not applicable
Case 1
A 71-year-old male with beta-thalassemia and hypertension presented with acute burning upper abdominal pain, fullness, nausea, vomiting, and constipation. Computed tomography (CT) demonstrated a thrombus in the PV, SMV, and distal branches with associated mesenteric edema. Symptoms did not improve with heparin drip. The patient had a distended abdomen with diffuse tenderness and hypoactive bowel sounds. The right internal jugular (IJ) vein was accessed, and venography showed a patent right hepatic vein. Subsequent indirect portography through the right hepatic vein demonstrated patent right and left PV branches, with a near occlusion of the main PV [Figure 1]. TIPS placement, balloon dilation, and thrombectomy of the SMV and PV were performed as described above. IVUS during TIPS placement was not feasible due to the profoundly echogenic liver due to hepatic steatosis. TIPS placement and subsequent thrombectomy resulted in a significant reduction in thrombus volume and restored outflow from the SMV [Figure 1]. At 2-month follow-up, symptoms had resolved, and the patient continued anticoagulation without complications.
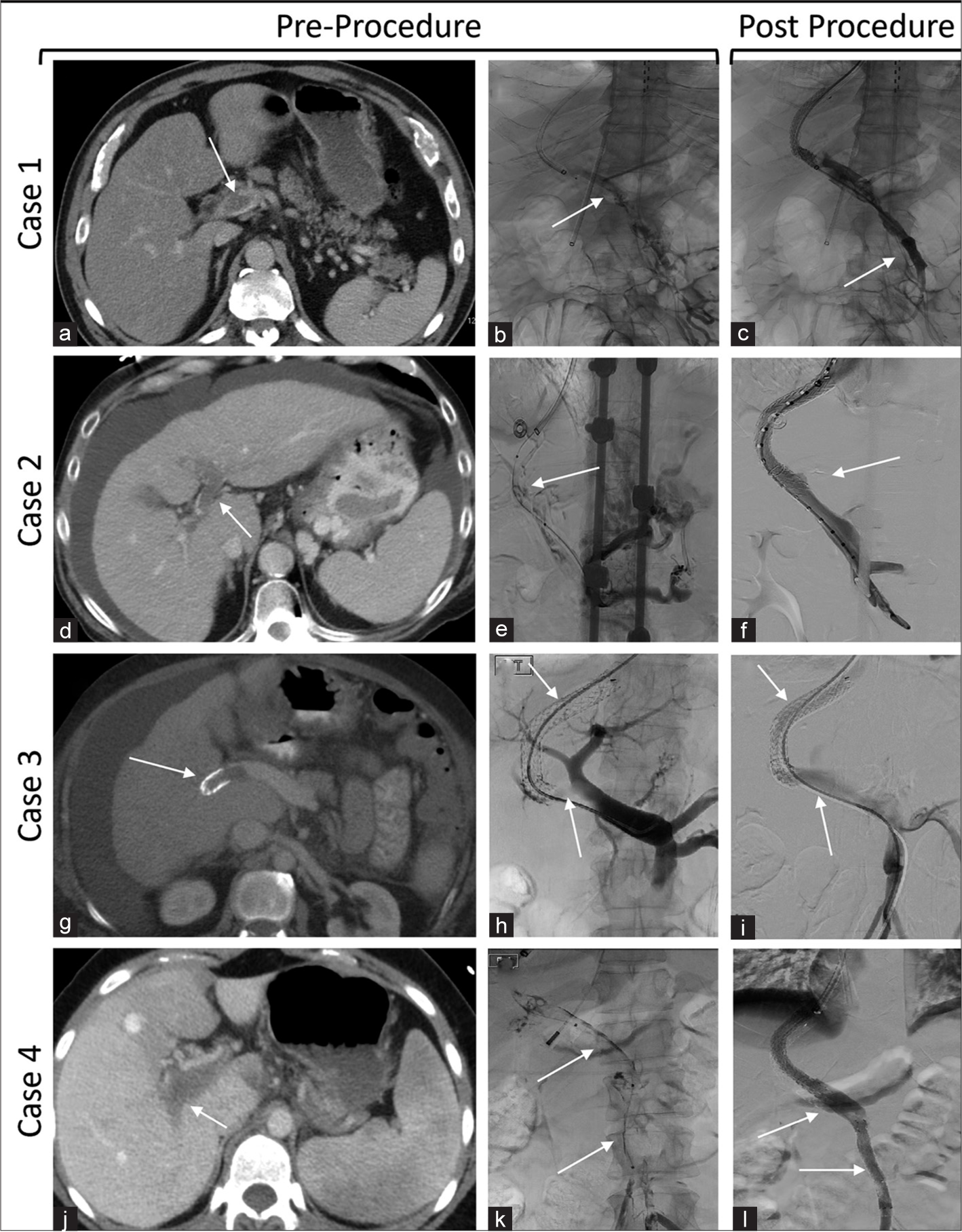
- Case 1 is a 71-year-old man who presented with abdominal pain and mesenteric vein thrombosis. (a) Pre-intervention CT of the portal system shows a thrombus in the PV (white arrow). (b) Portogram following transhepatic IVUS-guided access shows near occlusion of main PV (white arrow). (c) Post-intervention venography shows improved outflow from the SMV (white arrow). Case 2 is a 67-year-old man who presented with mesenteric vein thrombosis and variceal bleeding. (d) Pre-intervention CT of the abdomen shows thrombosed PV (white arrow). (e) Portogram following IVUS-guided portal venous access shows thrombosed main PV (white arrow). (f) Post-intervention venography shows patent PV (white arrow). Case 3 is a 62-year-old woman with cirrhosis, acute upper GI bleeding, and a thrombosed pre-existing TIPS. (g) Pre-intervention CT of the portal system shows thrombosed pre-existing TIPS (white arrow). (h) The portogram showed TIPS occlusion with a thrombus extending into the right and main PV (white arrows). (i) Post-intervention venography shows patent TIPS with restored hepatopetal flow (white arrows). Case 4 is a 25-year-old woman who presented with abdominal pain and mesenteric vein thrombosis. (j) Pre-intervention CT of the portal system shows thrombosed PV (white arrow). (k) Portography following IVUS-guided portal vein access demonstrated a thrombosed main PV and SMV (white arrows). (l) Post-intervention venography shows restored blood flow through the PV and SMV (white arrows). The bottom arrow indicates the stent placed in the SMV. (CT: Computed tomography; PV: Portal vein; SMV: Superior mesenteric vein, TIPS: Transjugular intrahepatic portosystemic shunt, IVUS: Intravascular ultrasound).
Case 2
A 67-year-old male with a history of nonalcoholic steatohepatitis with portal hypertension, congestive heart failure, chronic obstructive pulmonary disease, diabetes mellitus type 2, thrombocytopenia, and chronic opioid use presented with altered mental status, an upper gastrointestinal (GI) bleed, and a MELD score of 11. The patient was found to have elevated pro-BNP and an abnormal chest radiograph with findings concerning multifocal pneumonia versus pulmonary edema. During a recent hospital admission, he was found to have PVT, and apixaban was prescribed. Esophagogastroduodenoscopy showed large esophageal varices, erosive esophagitis, and severe portal hypertensive gastropathy. TIPS placement and PV thrombectomy were indicated by variceal bleeding. The right internal jugular (IJ) vein was accessed, and venography showed a patent right hepatic vein. Subsequent indirect portography through the right hepatic vein showed a thrombosed main PV. TIPS placement and thrombectomy of the main PV as described above resulted in the removal of a significant amount of chronic-appearing thrombus with no significant residual thrombus [Figure 1]. The patient was discharged to rehabilitation and expired after presenting with a myocardial infarction and pneumonia 2 weeks post-procedure.
Case 3
A 62-year-old female with alcohol-related chronic liver disease with portal hypertension and bleeding esophageal varices, gastric antral vascular ectasia (GAVE), recurrent GI bleed, hypertension, and chronic gastritis presented with abdominal pain, shortness of breath for 3 days, and a MELD score of 17. CT demonstrated occlusion of pre-existing TIPS with abdominal ascites and right pleural effusion [Figure 1]. She was not a candidate for anticoagulation given her history of GAVE and underwent endoscopy and argon plasma coagulation therapy 48 h before InThrill thrombectomy and initiation of anticoagulation. The PV was catheterized through the indwelling TIPS, and venography showed TIPS occlusion with a thrombus extending into the right and main PV [Figure 1]. A 16-French sheath was advanced to the cranial apex of the TIPS and the InThrill thrombectomy catheter was deployed in the SMV. The catheter was pulled through the occluded TIPS 4 times. The thrombectomy catheter was then deployed in the splenic vein and pulled through the TIPS once, followed by angioplasty using a 10 mm balloon. Venography showed a widely patent TIPS with restored hepatopetal flow [Figure 1]. An abdominal Doppler ultrasound at a 2-month follow-up demonstrated a patent TIPS [Figu re 2].
Case 4
A 25-year-old female without significant past medical history presented with severe abdominal pain for 6 days. The patient had been on oral contraceptive pills for 2 months. CT showed thrombosis of the PV, SMV, and distal branches. She completed 3 days of heparin drip without symptom improvement. Her D-dimer was elevated at 4.19 mg/L with lactic acid within normal limits. The right internal jugular (IJ) vein was accessed, and venography showed a patent right hepatic vein. Subsequent indirect portography through the right hepatic vein demonstrated a thrombosed main PV. TIPS placement, balloon dilation, and thrombectomy were performed as described above. Thrombectomy with InThrill removed a significant amount of acute and chronic thrombus, with less than 10% of the thrombus remaining. However, residual stenosis in the SMV and poor blood flow through the portal system led to the decision to perform venoplasty of the SMV with an 8 × 80 mm Mustang balloon (Boston Scientific, Marlborough, MA, USA) followed by placement of an 8 × 80 mm Epic stent (Boston Scientific, Marlborough, MA, USA). Subsequent blood flow was significantly improved throughout the SMV and portal system with no significant residual stenosis [Figure 1]. A CT scan and abdominal Doppler at 2-month follow-up showed maintained patency [Figure 2].

- Case 3 is a 62-year-old woman who presented with abdominal pain and shortness of breath for 3 days and was treated for TIPS thrombosis and acute upper GI bleed. (a) Color abdominal Doppler imaging at 2 months shows a widely patented TIPS (white arrow). Case 4 is a 25-year-old woman treated for symptomatic mesenteric vein thrombosis. (b) Two-month follow-up abdominal Doppler shows a patent TIPS (white arrow). (c and d) Two-month follow-up CT images show patent TIPS and SMV stents (white arrows). (PV: Portal vein, SMV: Superior mesenteric vein, CT: Computed tomography, TIPS: Transjugular intrahepatic portosystemic shunt, IVUS: Intravascular ultrasound, GI: Gastrointestinal).
DISCUSSION
TIPS placement can help alleviate portal hypertension by providing outflow to the PV as well as providing access to the portal system for endovascular devices.[2] While thrombolysis has been proposed as an adjunct to anticoagulation in cases of acute deep vein thrombosis (DVT), major complication rates as high as 60% have been associated with transcatheter thrombolysis.[6] Furthermore, the American Association for the Study of Liver D iseases (AASLD) recommends against thrombolytics due to high procedure-related morbidity and mortality and similar thrombus clearance rates as anticoagulation alone.[7]
Mechanical thrombectomy has been proposed as an alternate treatment option for thrombolysis; however, available devices have shown mixed results. A retrospective analysis of ten patients with PVT treated with the FlowTriever system (Inari Medical, Irvine, CA, USA) found that suction thrombectomy was effective on acute and subacute PVT.[8] However, a retrospective analysis of 32 patients who underwent mechanical thrombectomy for PVT with a variety of other devices found that 69% of patients required multiple devices, 63% required thrombolytics, and only 31% were treated in a single session.[9]
Using the newly available InThrill thrombectomy catheter, all patients were treated in a single session without thrombolytics, resulting in >90% removal of acute to chronic thrombus in all cases. There were no procedure-related complications. The average procedure time was 104 min. For the surviving patients, patency and symptom resolution were maintained at the 2-month follow-up.
Compared to the FlowTriever system, which worked well on acute and subacute PVT,[8] InThrill is a smaller profile option with a mechanism of action that may be more suitable for the mesenteric system. The 8-French InThrill system has a coring element with an integrated c ollection bag that can self-expand up to 18 mm allowing for full wall apposition in the mesenteric veins to mechanically disrupt and remove acute to chronic wall-adherent thrombus. The ClotTriever sheath aided in thrombus clearance by removing additional thrombus through aspiration after each InThrill pass. The ClotTriever catheter was not used to mechanically disrupt the thrombus as the coring element is too large for the mesenteric system. With additional studies, thrombectomy with InThrill may prove as an effective treatment option for PVT.
CONCLUSION
Mechanical thrombectomy with InThrill was feasible and effective in removing thrombus to restore patency in patients with PVT and occluded TIPS in a single session without thrombolytics. Long-term follow-up as well as additional studies are warranted to validate its long-term effectiveness.
Acknowledgments
We would like to thank Inari Medical (Irvine, CA, USA) for their medical writing assistance.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Derek Mittleider, MD is a consultant for Inari Medical.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Diagnosis, development, and treatment of portal vein thrombosis in patients with and without cirrhosis. Gastroenterology. 2019;156:1582-99.e1.
- [CrossRef] [PubMed] [Google Scholar]
- Portal vein thrombosis: Diagnosis and endovascular management. Rofo. 2022;194:169-80.
- [CrossRef] [PubMed] [Google Scholar]
- Early experience and key learnings of the inthrill thrombectomy system for treating arteriovenous access thrombosis in hemodialysis patients. Cath Lab Digest. 2023;31:1-7.
- [Google Scholar]
- Single sweep transjugular thrombectomy (Declot) of a hemodialysis graft using the inthrill thrombectomy system. Cardiovasc Intervent Radiol. 2023;46:686-8.
- [CrossRef] [PubMed] [Google Scholar]
- Novel percutaneous mechanical thrombectomy device for treating upper extremity deep vein thrombosis in patient with paget-schroetter syndrome. Vasc Endovascular Surg. 2024;58:235-239.
- [CrossRef] [PubMed] [Google Scholar]
- Transcatheter thrombolytic therapy for acute mesenteric and portal vein thrombosis. J Vasc Interv Radiol. 2005;16:651-61.
- [CrossRef] [PubMed] [Google Scholar]
- Vascular liver disorders, portal vein thrombosis, and procedural bleeding in patients with liver disease: 2020 practice guidance by the American association for the study of liver diseases. Hepatology. 2021;73:366-413.
- [CrossRef] [PubMed] [Google Scholar]
- Large bore portal vein thrombectomy: An inari flowtriever case series. Cardiovasc Intervent Radiol. 2023;46:136-41.
- [CrossRef] [PubMed] [Google Scholar]
- Transjugular intrahepatic portosystemic shunt creation and thrombectomy for symptomatic acute non-cirrhotic portal vein thrombosis. J Vasc Interv Radiol. 2023;34:1373-81.e3.
- [CrossRef] [PubMed] [Google Scholar]






