Translate this page into:
Vacuum-assisted thrombectomy of a right atrial vegetation in a patient with infective endocarditis

*Corresponding author: MacKenzie Mayo, Department of Internal Medicine, Trinity Health Ann Arbor Hospital, Ypsilanti, United States. mackenzie.mayo@trinity-health.org
-
Received: ,
Accepted: ,
How to cite this article: Mayo M, Manley-Casco D, Girard S, Sarosi M. Vacuum-assisted thrombectomy of a right atrial vegetation in a patient with infective endocarditis. Am J Interv Radiol 2022;6:12.
Abstract
Infective endocarditis has a high mortality rate despite appropriate medical therapy. In patients who are not surgical candidates, source control can be achieved with less invasive intervention. This case report describes a 47-year-old male with a complex medical history who presented in septic shock with recurrent bacteremia. Transesophageal echocardiogram showed the right atrial septal vegetation, but multiple medical comorbidities rendered the patient a poor surgical candidate. He underwent successful vacuum-assisted thrombectomy with the FlowTriever System™ (Inari Medical, Inc.) and was discharged home 6 days after the procedure. Intervention with this device can provide life-saving therapy in critically ill patients.
Keywords
Endocarditis
Vegetation
Vacuum-assisted thrombectomy
FlowTriever System
Right atrial vegetation
Septal vegetation
INTRODUCTION
Infective endocarditis is a life-threatening condition with an incidence of 10,000–15,000 cases per year in the United States, and mortality is high even with appropriate medical therapy.[1] Classical therapy for infective endocarditis includes a prolonged antibiotic course and source control, which is often achieved surgically. Early surgical intervention is indicated particularly for patients with heart failure or uncontrolled infection.[2] However, surgical intervention is not always possible, so other less invasive interventions may provide life-saving therapy. This report describes a patient with a right atrial septal vegetation who underwent vacuum-assisted thrombectomy (VAT) with the FlowTriever System™ (Inari Medical, Inc.), specifically using the Triever24™ aspiration catheter, which led to successful source control and clinical improvement.
CASE REPORT
The patient is a 47-year-old male with a history of autosomal dominant polycystic kidney disease status post bilateral nephrectomy on hemodialysis; short gut syndrome due to small bowel resection and hemicolectomy on total parenteral nutrition; heart failure with preserved ejection fraction of 48%; coronary artery disease status post three-vessel coronary artery bypass grafting; and recent admission for septic shock due to presumed central line-associated blood stream infection (CLABSI) secondary to his hemodialysis (HD) catheter in the internal jugular vein. He returned to the emergency department 2 weeks after his previous discharge with altered mental status and was re-admitted to the medical intensive care unit (MICU) with recurrent septic shock requiring multiple pressors. CTA chest and CT abdomen/ pelvis showed pleural effusion and multiple pulmonary septic emboli, but no clear source of infection. Blood cultures drawn on presentation were positive for Citrobacter koseri and Pseudomonas aeruginosa, consistent with cultures from the previous admission. Pleural fluid culture was negative. Transesophageal echocardiography (TEE) was obtained due to concern for IE, and it showed a 3.0 × 1.7 cm mobile right atrial upper septal vegetation but no atrial septal defect and no valve involvement. Given his history of recurrent bacteremia and previous CLABSI, the vegetation was most likely due to the HD catheter. The tip was appropriately positioned within the right atrium to expose it to the most turbulent flow, which avoids but does not preclude thrombus formation.
Surgical removal of the vegetation was not offered due to the patient’s multiple severe comorbidities and poor surgical candidacy. Interventional radiology was consulted and source control was achieved thorugh a successful, uncomplicated percutaneous VAT using the FlowTriever System. Following intravenous conscious sedation with Fentanyl and Versed, ultrasound guidance was used to access the right femoral vein and a 5 F Kumpe catheter and 0.035 inches Glidewire combination was used to reach the right brachiocephalic vein. The Glidewire was then exchanged for a 0.035 Amplatz Super Stiff wire with a 1 cm taper. The femoral vein was dilated and 24 F Dry-Seal sheath placed. The Triever24 catheter was advanced through the sheath under intermittent fluoroscopic guidance up to the IVC/right atrial junction. At that point, continual subcostal transthoracic echocardiography (TTE) guidance was used to guide the Triever24 up to the visible vegetation [Figure 1]. The vegetation was extracted on the first aspiration [Figure 2]. A second aspiration was performed to confirm no additional vegetation remained, and none was retrieved. TTE confirmed that no residual vegetation remained. Total procedure time was 31 min with estimated fluoroscopic time of 1.7 min. Estimated blood loss was 100 cc.
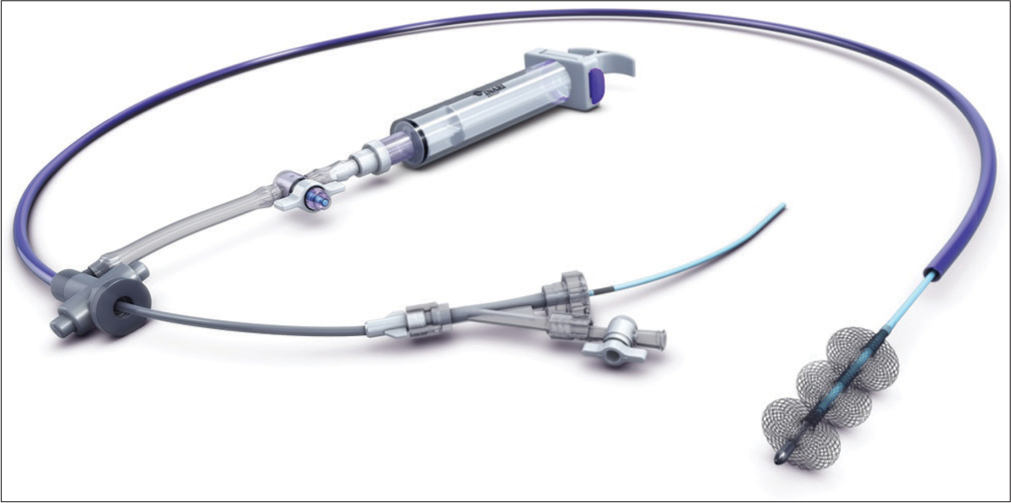
- A 47-year-old male who presented in septic shock with bacteremia and was found to have infective endocarditis with a right atrial septal vegetation. This digital illustration shows the Inari Medical FlowTrieverTM, consisting of a catheter and aspiration system that was used in the vacuum-assisted thrombectomy of the vegetation for this patient.

- A 47-year-old male who presented in septic shock with bacteremia and was found to have infective endocarditis with a right atrial septal vegetation. Transthoracic echocardiographic guidance during the thrombectomy procedure showed the right atrial septal vegetation, which measured 3 × 1.7 cm. The green markers indicate the measurement of the vegetation.
Culture of the right atrial vegetation was positive for C. koseri and P. aeruginosa [Figures 3 and 4]. After the procedure, the patient maintained hemodynamic stability without pressors and did not have a recurrent septic event; he was transferred out of the MICU the next day. Repeat blood cultures after VAT and line exchange were negative. Antibiotics were deescalated to cefepime, and the patient was discharged home in stable condition 6 days post-procedure with a plan to complete a total antibiotic course of at least 6 weeks. Weekly laboratories were obtained after discharge which showed initial rise and then drop in inflammatory markers. He was seen in follow-up at the infectious diseases clinic 3 weeks after discharge. Repeat transthoracic echocardiograms at 4 weeks and 8 weeks post-procedure showed resolution of the right atrial septal vegetation and he completed the antibiotic course without complication. In follow-up over the next several months, the patient had two additional admissions. The first was to the surgical ICU for a small bowel obstruction secondary to his history of multiple abdominal surgeries; the obstruction resolved without surgical intervention. The second admission was to the medical ICU for sepsis due to bacteremia with blood cultures positive for Escherichia coli. Transthoracic echocardiogram was negative for vegetations and the patient completed a 10-day course of ceftriaxone.

- A 47-year-old male who presented in septic shock with bacteremia and was found to have infective endocarditis with a right atrial septal vegetation. Photograph shows the two fragments that comprised the right atrial septal vegetation that was removed through vacuum-assisted thrombectomy.

- A 47-year-old male who presented in septic shock with bacteremia and was found to have infective endocarditis with a right atrial septal vegetation. H&E stain of the right atrial septal vegetation at 200 × magnification shows layers of neutrophilic debris at the bottom of the image, fibrin and bacteria in the middle, and fibrin and neutrophils at the top.
DISCUSSION
Sepsis due to IE can be life-threatening; the mortality rate remains very high despite appropriate medical therapy and increases with age and number of comorbidities.[3] In patients with end-stage renal disease requiring HD, the mortality rate can reach 43.1%.[4] Surgical management, when indicated, becomes problematic in elderly and critically ill patients due to the increased risks inherent to the operative approach. There are currently no guidelines, however, regarding minimally invasive approaches to achieve source control in these patients. New percutaneous interventional devices, including the FlowTriever System™ and the AngioVac System (AngioDynamics, Inc.), have shown promising utility as a minimally invasive approach to achieving source control in the treatment of IE.[2] The percutaneous approach may allow for favorable outcomes in patients with IE who are critically ill or those with multiple comorbidities who are deemed poor candidates for an open-heart procedure.[5] It also allows for faster recovery and shorter hospital stay.[6]
To the authors’ knowledge, VAT for the right atrial septal vegetation using the FlowTriever System has not been previously reported. The FlowTriever System has demonstrated success in VAT for tricuspid valve endocarditis,[7] pulmonary embolism,[8] and right atrial clot-in-transit.[9,10] These percutaneous endovascular VAT procedures can be performed under guidance of various sonographic imaging modalities, including transesophageal and TTE,[9,10] and can be performed without the need for cardiopulmonary bypass to simplify procedural support requirements.
Given the utility of the FlowTriever System in this case, its demonstrated use for the right atrial clot-in-transit,[8,9] and the recent introduction of the new curved, steerable Triever20 Curve™ aspiration catheter, this technique may provide an even less invasive approach than the AngioVac System. The AngioVac System has been used previously for removal of the right-sided atrial and valvular vegetations, and atrial and caval venous thrombi.[5,6,11] However, the AngioVac System utilizes an extracorporeal bypass filtration method requiring two percutaneous cannulas; the FlowTriever System uses a single percutaneous entry site and an aspiration system that minimizes blood loss. One caveat is that when using the FlowTriever System, the practitioner must be both skilled and prepared for the possibility of vegetation embolization into the pulmonary artery, with possible hemodynamic decompensation and the need to pursue VAT in the pulmonary artery to extract the embolized vegetation. Previously reported complications include hemoptysis,[12] blood loss,[12] and cardiac tamponade due to cardiac wall perforation.[13]
IRB approval was not required for this case report.
CONCLUSION
Mortality due to IE is high and surgical intervention often carries significant risk due to patients’ hemodynamic instability and medical comorbidities. VAT is an alternative therapy that can provide source control without exposing the patient to surgical risk and has shown initial success in improving outcomes for these patients. This report describes the first known use of the FlowTriever System for VAT extraction of a right atrial septal vegetation. Additional studies are warranted to further investigate and develop guidelines regarding its use.
Acknowledgments
The authors thank Jessi Parsons for help in manuscript editing.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Mortality from infective endocarditis: Clinical predictors of outcome. Heart. 2002;88:53-60.
- [CrossRef] [PubMed] [Google Scholar]
- Infective endocarditis-a review of current therapy and future challenges. Hellenic J Cardiol. 2021;62:190-200.
- [CrossRef] [PubMed] [Google Scholar]
- Role of age and comorbidities in mortality of patients with infective endocarditis. Eur J Intern Med. 2019;64:63-71.
- [CrossRef] [PubMed] [Google Scholar]
- Inhospital and long-term outcomes of infective endocarditis in chronic dialysis patients. Int J Gen Med. 2021;14:425-34.
- [CrossRef] [PubMed] [Google Scholar]
- Using aspiration-based tricuspid valve endocarditis debridement: Highlighting imaging-based modification in a high-risk clinical scenario. JACC Case Rep. 2019;1:742-5.
- [CrossRef] [PubMed] [Google Scholar]
- AngioVac for extraction of venous thromboses and endocardial vegetations: A meta-analysis. J Card Surg. 2019;34:170-80.
- [CrossRef] [PubMed] [Google Scholar]
- A novel technique for the percutaneous removal of tricuspid valve vegetations utilizing the Inari Flowtriever System. Catheter Cardiovasc Interv. 2022;100:261-5.
- [CrossRef] [PubMed] [Google Scholar]
- A prospective, single-arm, multicenter trial of catheter-directed mechanical thrombectomy for intermediate-risk acute pulmonary embolism: The FLARE Study. JACC Cardiovasc Interv. 2019;12:859-69.
- [CrossRef] [PubMed] [Google Scholar]
- Catheter directed embolectomy of right atrial clot in transit-a case series. Catheter Cardiovasc Interv. 2021;97:869-73.
- [CrossRef] [PubMed] [Google Scholar]
- Right atrial and massive pulmonary artery mechanical thrombectomy under echocardiography guidance using the FlowTriever System. EJVES Short Rep. 2019;45:22-5.
- [CrossRef] [PubMed] [Google Scholar]
- Endovascular removal of thrombus and right heart masses using the AngioVac System: Results of 234 patients from the prospective, multicenter registry of AngioVac procedures in detail RAPID. J Vasc Interv Radiol. 2021;32:549-57.e3.
- [CrossRef] [PubMed] [Google Scholar]
- Safety and efficacy of acute pulmonary embolism treated via large-bore aspiration mechanical thrombectomy using the Inari FlowTriever device. J Vasc Interv Radiol. 2019;30:1370-5.
- [CrossRef] [PubMed] [Google Scholar]
- A novel case of cardiac tamponade after percutaneous pulmonary embolectomy using the FlowTriever Retrieval/Aspiration System. Eur J Case Rep Intern Med. 2022;9:003522.
- [Google Scholar]






