Translate this page into:
The Modified Lateral Approach: Experience of a Single Center using an Alternative Technique to Conventional Transpedicular Percutaneous Vertebroplasty

Corresponding Author: Isabelle Dupuis, Department of Radiology, McGill University, Montreal General Hospital, Rm C5 118, 1650 Cedar Avenue, Montreal, QC, H3G 1A4, Canada. E-mail: isabelle.dupuis2@mail.mcgill.ca
-
Received: ,
Accepted: ,
How to cite this article: Dupuis I, Forghani R, Le H. The Modified Lateral Approach: Experience of a Single Center using an Alternative Technique to Conventional Transpedicular Percutaneous Vertebroplasty. Am J Interv Radiol 2019;3(6):1-7.
Abstract
Objective:
The objective of this study was to assess whether the placement of a needle more lateral to the pedicle while using a transpedicular approach compared to the conventional technique yields comparable or better vertebral body filling.
Methods:
Retrospective review of 134 thoracic and lumbar unipedicular vertebroplasties performed by a single radiologist (110 lateral and 24 classic). Vertebral bodies were divided into eight voxels on computed tomography and the percent of coverage was documented. 50% and 75% cement filling thresholds were defined as “efficient.” Complications were retrospectively collected. Chi-square (χ2) was used to compare the filling efficacy and rates of extravertebral cement leakage between the approaches. Bivariate analysis was performed to assess variables potentially influencing the efficacy.
Results:
There was no significant difference between the two approaches for 50% coverage (classic; n = 21 [87.5%] vs. lateral; n = 98 [89.1%], P = 0.8228). There was more efficient coverage >75% using the lateral approach (classic; n = 4 [16.7%] vs. lateral; n = 46 (41.8%), P = 0.0210). Vertebral body level (50.8% thoracic vs. 26.0% lumbar, P = 0.0031) and fracture type (45.6% pathological vs. 29.2% osteoporotic, P = 0.0444) were associated with 75% coverage. Three classic cases (12.5%) had extravertebral cement leakage versus 34 lateral cases (30.9%), which was not statistically significant (P = 0.0676). Other complications included one asymptomatic lung embolization using both approaches, one pedicular fracture using the classic approach, and one overnight admission for analgesia using the lateral approach.
Conclusion:
A modified lateral approach proved to be as safe and more effective in achieving 75% or more vertebral filling in treating compression fractures compared to the conventional approach.
Keywords
Vertebroplasty
Transpedicular
Vertebral body filling
INTRODUCTION
The technical aspects of percutaneous vertebroplasty (PV) have been widely studied. A unilateral, transpedicular approach yields good results and reduced procedural time with no significant difference compared with a bilateral approach.[1,2] A transpedicular approach is preferred, as a parapedicular approach is associated with higher complication rates.[3,4] The commonly described technique for thoracic and lumbar transpedicular access is with the needle entering the pedicle in the upper outer quadrant when the pedicle is seen “en face.” Having the needle in the upper outer quadrant allows the operator to steer the needle as medially as possible without breaching the medial cortex, which delineates the critical boundary with the spinal canal. The needle is advanced until the tip has reached the anterior and inferior third of the vertebral body on a lateral view. The optimal final positioning of the needle is such that the tip lies in the midline of the vertebra, which should allow homogeneous filling. This technique is considered safe and effective. However, it is associated with a potential risk, though very small, of breaching the medial pedicular cortex and entering the spinal canal.
At our institution, multiple vertebroplasties have been performed using the classic approach. However, the anatomy of the pedicle from patient to patient varies, and thus, good cortical purchase with a beveled needle is not always possible. Furthermore, with the classical technique, there is sometimes insufficient space in the pedicle to navigate the needle safely while trying to park the needle tip at the midline of the vertebral body. This is often encountered in patients with long and/or narrow pedicles. This has led us to make modifications to the classical approach – repositioning the needle slightly more lateral to the pedicle under fluoroscopy, while remaining transpedicular has allowed better cortical purchase and a more central final position in the vertebral body. This lateral approach (hereafter referred to as modified lateral approach) also has the advantage of a theoretical lower risk of breaching the medial pedicular cortex.
The purpose of this study was to evaluate the use for a modified lateral transpedicular approach and compare it to the classical approach. Our hypothesis is that the technique provides a higher rate of satisfactory filling of the vertebral body with cement compared to the classical approach with comparable or lower rates of periprocedural complications.
MATERIAL STUDIED, AREA DESCRIPTIONS, METHODS, AND TECHNIQUES
This project was reviewed and approved by the Research Ethics Committee of our institution. Access to picture archiving and communication system (PACS) was approved and patient identifiable information was removed.
Patient population
A retrospective review of all thoracic and lumbar unipedicular vertebroplasties performed between October 2009 and January 2016 by a single experienced musculoskeletal-trained radiologist with 9 years of experience was performed. 140 treated levels were found. 66 osteoporotic and 68 pathologic compression fractures were included. There were two traumatic fractures and four redo interventions which were excluded.
Procedure details
Unipedicular procedures using both the classic and the modified lateral approach were included (Figures 1-3). The rationale of the procedure as well as the details, risks, and expectations was explained by the radiologist before informed consent was obtained. All patients received a prophylactic dose of systemic intravenous antibiotics (1 g cefazolin or 400 mg ciprofloxacin) before initiating the procedure. All cases were performed under conscious sedation using intravenous fentanyl and midazolam and patients were continuously monitored with the assistance of a nurse. Patients were placed prone with a pillow under their abdomen for comfort. Local anesthesia (1% xylocaine) was administered regionally for the overlying soft tissues and directly over the pedicle cortex, followed by a 5 mm vertical incision. The frontal projection was obtained first, by rotating the C-arm 30–45° obliquely until the pedicle was seen directly and the medial cortex was best visualized. For each procedure, a 10 cm or 15 cm beveled 13G Osteo-Site® (CookTM, IN, USA) bone biopsy needle was used to access the vertebral body. Initially, the needle was placed at the upper outer quadrant of the pedicle (for a classic approach) such that the bevel was facing laterally. For a modified lateral approach, the needle was placed 1–2 mm lateral to the upper outer margin of the pedicle. With the bevel facing outward in both techniques, this allowed a superior cortical purchase in the pedicle and also allowed the needle to steer medially. The needle was angled between 20 and 45° from the midline, depending on the patient’s anatomy, before being advanced into the pedicle using a mallet. Positioning of the needle was confirmed at all times with frontal and lateral projections. The goal was to navigate the needle safely through the pedicle, while keeping a medial trajectory and simultaneously avoiding breaching the medial cortex. The medial trajectory would allow an optimal final midline position of the needle tip in the anterior and inferior third of the vertebral body. In cases where the needle tip was encroaching on the medial pedicle cortex before passing through the pedicle, the bevel was turned medially to allow the needle safely steer away from the medial cortex. Once the needle was safely past the pedicle (confirmed on a true lateral view), the needle was angled as much as possible (with the bevel facing outward) to steer the needle toward the midline of the vertebral body. The final position of the needle was in the anterior and inferior third of the vertebral body. Spinal cement systems by Cook™ (IN, USA) were utilized for cement augmentation. Cement was injected until there was either satisfactory coverage of the vertebral body or cement was seen encroaching on the basivertebral venous plexus/central canal epidural space. In some cases, more than one level was treated, with a maximum of three levels treated per session. After the procedure, direct pressure was applied until hemostasis was achieved. Outpatients were then observed for 4 h post-procedure before being allowed to ambulate. This time allowed optimal pain management and cement curing before the patient could be discharged. Admitted patients returned to their specified ward with detailed post-procedure orders filled out by the radiologist. All patients had pre-arranged follow-up appointments with their referring physicians.
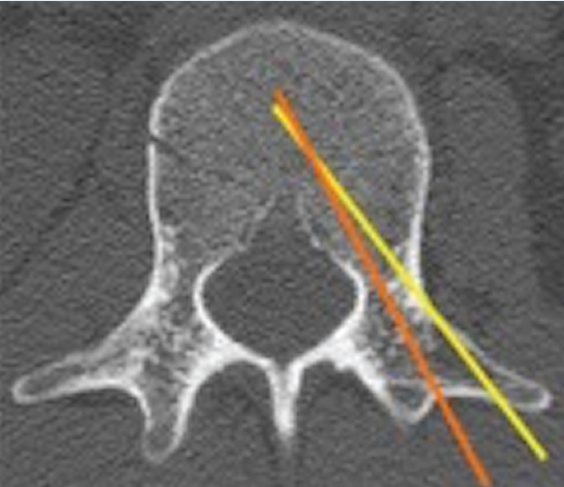
- Axial computed tomography of the thoracic spine centered at T12 in a 56-year-old female without pathology involving the thoracic spine demonstrating a left-sided transpedicular needle trajectory using the modified lateral approach (yellow line) and classic approach (orange line).

- A 72-year-old male with multiple myeloma presenting with back pain and a compression fracture of the T7 vertebral body on computed tomography (CT) of the thoracic spine. Thoracic vertebroplasty for the treatment of an osteoporotic compression fracture of the thoracic spine using the classic approach. (a) Post-procedural axial CT in bone window demonstrating the needle tract into the left pedicular cortex which was entered centrally. (b) Post-procedural axial CT in bone window in the same patient demonstrating the central access of the needle tract (arrow) in the vertebral body.

- A 65-year-old male with osteoporosis presenting with back pain and a compression fracture of the T9 vertebral body on computed tomography (CT) of the thoracic spine. Thoracic vertebroplasty for the treatment of a pathologic compression fracture using the modified lateral approach. (a) Post-procedural axial CT in bone window demonstrating the needle tract (arrow) with a slightly more left lateral pedicular access with a needle puncture just lateral to the pedicle. (b) Post-procedural axial CT in bone window in the same patient demonstrating the left intrapedicular needle tract (arrow). (c) Post-procedural axial CT in bone window in the same patient demonstrating central access of the needle tract (arrow) in the vertebral body.
Imaging review
Static fluoroscopic images were saved during the procedure. For each case, a non-infused computed tomography (CT) of the spine including the treated level(s) was performed immediately after the procedure. The CT images were used to confirm the needle positioning and pedicle purchase site (modified lateral vs. classic approach), to evaluate the filling of the vertebral body with cement, and to serve as a baseline examination for future follow-ups.
Vertebral body filling measurement
The vertebral body coverage with cement was evaluated using the post-procedure CT. The vertebral body was divided into eight voxels and the percent of voxel coverage by the cement into the vertebral body was documented (Table 1). Cases with extravertebral cement leakage were also all recorded.
| Position | Location | ||
|---|---|---|---|
| 1 | Superior | Anterior | Left |
| 2 | Superior | Anterior | Right |
| 3 | Superior | Posterior | Left |
| 4 | Superior | Posterior | Right |
| 5 | Inferior | Anterior | Left |
| 6 | Inferior | Anterior | Right |
| 7 | Inferior | Posterior | Left |
| 8 | Inferior | Posterior | Right |
Complications
All periprocedural complications were detailed. Patients were also instructed to call the performing radiologist if symptoms were encountered following the procedure. All periprocedural complications were retrospectively collected.
Statistical analysis
We evaluated vertebral body filling using two different thresholds of vertebral body filling (≥50% and ≥75% of voxels). For the purpose of this study, these thresholds were defined to be “efficient.” Pearson’s Chi-squared test (χ2) was used to compare the efficacy of the classic and modified lateral approach. Bivariate analysis was performed to assess possible variables influencing the efficacy of vertebral body filling, including:
-
Age
-
Sex
-
Vertebral body level (thoracic vs. lumbar spine)
-
Type of fracture (osteoporotic vs. pathologic)
-
Type of malignancy
-
Needle position in the vertebral body (midline or not midline).
A Student’s t-test was used to assess the age and the other variables were assessed using a Chi-squared test (χ2). The two approaches were also compared in terms of extravertebral MMA leakage using a Chi-squared test (χ2).
RESULTS
Among our initial cohort of 140 levels, four levels were excluded as they were redo interventions (these levels had <25% coverage initially and were still symptomatic which required a repeat intervention on a separate day with puncture on the contralateral pedicle). Two traumatic fractures were also excluded as they occurred in much younger and healthier patients without underlying osteoporosis or malignancy. A total of 134 vertebral body levels were included; 24 using the classing approach and 110 using the modified lateral approach. The descriptive summary of all the vertebroplasties performed is tabulated in Table 2. We have noticed that in cases where the lateral approach was used, this yielded a midline final position of the needle in the vertebral body in more than 85% of cases.
| Category | Lateral n=110(%) | Classic n=24(%) |
|---|---|---|
| Sex | ||
| Male | 40(36.4) | 12(50.0) |
| Female | 70(63.6) | 12(50.0) |
| Vertebral body level | ||
| Thoracic | 55(50.0) | 6(25.0) |
| Lumbar | 55(50.0) | 18(75.0) |
| Type of fracture | ||
| Osteoporotic | 54(49.1) | 12(50.0) |
| Multiple myeloma | 42(38.2) | 9(37.5) |
| Other malignancy | 14(12.7) | 3(12.5) |
| Needle position | ||
| Midline | 95(86.4) | 17(70.8) |
| Not midline | 15(13.6) | 7(29.2) |
Vertebral body coverage
All cases recorded had a coverage ≥25% of the vertebral body. Based on these observations, ≥50% and ≥75% coverage thresholds were used to calculate any statistical difference in filling efficacy between the classical and modified lateral techniques.
a) ≥50% coverage
When using ≥50% cement coverage as the threshold for efficacy, there was no statistically significant difference between the two approaches: Classic; n = 21 (87.5%) versus lateral; n = 98 (89.1%), P = 0.8228 (Table 3).
Table 3: Efficacy of vertebral body filling using ≥50% and ≥75% coverageVertebral body filling Lateral n=110(%) Classic n=24(%) P value ≥50 98(89.1) 21(87.5) 0.8228 ≥75 46(41.8) 4(16.7) 0.0210 No variable had a statistically significant association with vertebral body filling ≥50% (Table 4).
Table 4: Variables influencing vertebral body fillingCategory ≥50% n=119 P value ≥75% n=50 P value Sex Male 46(88.5) 0.9198 19(36.5) 0.8826 Female 73(89.0) 31(37.8) Vertebral body level Thoracic 57(93.4) 0.1197 31(50.8) 0.0031 Lumbar 62(84.9) 19(26.0) Type of fracture Osteoporotic 56(86.2) 0.1523 19(29.2) 0.0444 Pathologic 63(92.7) 31(45.6) Malignancy type No malignancy 56(84.9) 0.2875 19(28.8) 0.1206 Multiple myeloma 48(94.1) 24(47.1) Other 15(88.2) 7(41.2) Needle position Midline 102(91.1) 0.0606 45(40.2) 0.1218 Not midline 17(77.3) 5(22.7) b) ≥75% coverage
When using ≥75% cement coverage as the threshold, there was a statistically significant difference between the two approaches: Classic; n = 4 (16.7%) versus lateral; n = 46 (41.8%), P = 0.0210 (Table 3).
Two variables were statistically associated with coverage ≥75%; vertebral body level and type of fracture (Table 4). There was more vertebral body coverage in the thoracic spine compared to the lumbar spine (50.8% of cases vs. 26.0% of cases, P = 0.0031). There was also better coverage in pathological fractures compared to osteoporotic fractures 45.6% of cases versus 29.2% of cases, P = 0.0444.
Technical events and complications
Among all the classical approaches, 3 cases (12.5%) had extravertebral MMA leakage; 2 (8.3%) extravasated in the intervertebral disc space and 1 (4.2%) extravasated into the basivertebral venous plexus. Among all the lateral approaches, 34 cases (30.9%) had extravertebral MMA leakage; 20 (18.2%) extravasated in the intervertebral disc space, 10 (9.1%) extravasated into the basivertebral venous plexus, and 4 (3.6%) extravasated in both the disc space and venous plexus. There was a higher trend toward higher MMA leakage using the lateral approach, but this was not significant (P = 0.0676).
One patient in whom three levels were treated had embolization of a small amount of MMA to the lungs, documented on a non-infused CT performed after the procedure. Two of the levels were treated using the classic approach and one was treated using the modified lateral approach. Determination of the level which resulted in embolization was not possible using the imaging modalities available. The two techniques could thus not be compared in terms of embolization risk. The patient was asymptomatic and there was no other associated morbidity.
In one patient who underwent a single lumbar insufficiency vertebral fracture treated with the classic approach, a non-displaced fracture of the punctured pedicle was recorded on the post-procedural CT. The fracture was treated conservatively.
Another patient with multiple myeloma with two levels treated (one thoracic and one lumbar) using the lateral approach required overnight admission for pain control. The patient was discharged the following morning with no subsequent complications.
DISCUSSION
The different technical aspects of PV have been studied and modified overtime, to ensure that it is a safe and efficient procedure with the goal of providing pain relief for patients with symptomatic vertebral body compression fractures. Only a few studies have evaluated the efficacy and safety of the unilateral transpedicular approach.[5]
Our study demonstrated that the modified lateral approach for a unipedicular vertebroplasty is as at least as effective as the classical approach for vertebral body filling ≥50% and more effective for ≥75% coverage of the vertebral body. However, there is little supporting or conflicting data showing a direct correlation between the percentage of vertebral body coverage improved clinical outcomes. One study demonstrated no correlation between the percentage of lesion filling and pain relief in patients with osteolytic metastases and multiple myeloma.[6] Some attempts have been made to evaluate the effect of cement filling in ex vivo biomechanical studies using osteoporotic cadavers, but to date, further studies are needed to evaluate the risk of refracture, complications, and benefits associated with the degree of cement filling.[7,8] Some centers advocate for a guideline to fill 50–70% of the residual volume of the compressed vertebra.[3]
Two variables were statistically associated with ≥75% vertebral body filling in our study. There was more vertebral body coverage in the thoracic spine compared to the lumbar spine. There was also better coverage in pathological fractures compared to osteoporotic fractures in our study. We speculate that the destruction of vertebral body trabeculae by tumor cells facilitates the spreading and percolation of cement within the vertebral body.
Low rates of complications have been associated with PV. Previous randomized controlled trials have not found significant increases in adverse outcomes with vertebroplasty.[9-11] The modified lateral approach had no mortality or life-threatening complications and any complications were not significantly higher than the classical approach. One case of post-procedural non-displaced pedicle fracture was reported with the classic approach and no fracture associated with the modified lateral approach. A meta-analysis by Han et al. did not support the hypothesis that vertebroplasty contributes to increased risk of subsequent vertebral fracture.[12]
Studies have shown that extravertebral MMA leakage into the disc space and basivertebral venous plexus is encountered in up to approximately 70% of cases, and in most cases are asymptomatic.[13] With the modified lateral approach, 30.9% had minor leakage but were all asymptomatic. This is in agreement with literature. Cotten et al. also demonstrated that discal and paravertebral leak had no clinical significance.[6]
The risk of a pulmonary cement embolism from PV ranges from approximately 3.5% to 23% for osteoporotic fractures.[14] Although we reported only one case of cement embolization to lungs for which both approaches were used, our results are aligned with literature for risk of cement embolization. Only rare isolated cases of symptomatic pulmonary cement embolism have been reported.[15] A study by Venmans et al. showed that clinically silent pulmonary cement emboli occurred in a quarter of their treated patients and that with time, these small cement emboli remained inert, without inflammatory pulmonary response.[16] Thus, routine thoracic imaging after vertebroplasty is usually not recommended and we are in agreement with literature.
One patient with two levels treated in our study required overnight admission for pain control. No complication such as MMA leakage or fracture was recorded for this patient. There is no clear documentation of the frequency of immediate post-procedural pain in PV in literature. Only one study by Ryu et al. demonstrated that epidural leakage of MMA may decrease the immediate therapeutic effects of vertebroplasty.[17] However, this was not our experience with our cases of extravertebral leakage, as none demonstrated a significant increase in immediate post-procedural pain.
Our study had several limitations. In addition to its retrospective design, the sample size of classical cases was much smaller compared to the modified lateral cases. This can potentially confound comparison between the two approaches. Furthermore, in the absence of three-dimensional volumetric analysis software, vertebral body filling could only be estimated using voxels. The reason is that the cement filling morphology was irregular and using conventional spherical volumetric calculations could not be done as such software was not available in the PACS used. There are no validated standardized methods to calculate vertebral body filling, and the voxel system used in this study has not yet been validated. The degree of compressive deformity has not been accounted for between 2 groups, which is also a limitation of the study. The primary objective of the study was to document vertebral body coverage with MMA using the modified lateral approach. This study did not assess the relationship between vertebral body filling and clinical outcomes such as pain relief and improved mobility. The benefits of PV have been widely studied in literature. The procedure has been shown to be superior to placebo in the recent vertebroplasty for acute painful osteoporotic fractures trial in patients with acute osteoporotic spinal fractures of <6 weeks in duration.[18] We hypothesize that the modified lateral technique would result in similar positive clinical outcomes as it provided higher rates of ≥75% filling compared to the classic approach. Additional limitation to this study was that the degree of vertebral body compression was not accounted in the analysis. Higher compression theoretically may restrict percolation of cement due to more condensed trabeculations and increased marrow pressures. This study also did not specifically assess clinical relief from vertebroplasty. Anecdotally, the vast majority of patients improved clinically, but we are unable to assess for a therapeutic difference between degrees of cement filling. This would be of interest to evaluate in the future.
Whether or not our results translate into improved clinical outcomes cannot be concluded and were not specifically assessed in this study. Only two studies thus far have shown a positive relationship between vertebral body filling and pain relief.[19,20]
CONCLUSION
The use of a modified lateral approach proved to be as safe and potentially more effective (in achieving 75% or more vertebral body filling) in treating compression fractures compared to the traditional classic approach. More studies assessing the relationship of vertebral body filling and clinical response will provide more detailed insight into the technical aspects of vertebroplasty.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Unilateral transpedicular percutaneous vertebroplasty: Initial experience. Radiology. 2002;222:737-41.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical outcomes with hemivertebral filling during percutaneous vertebroplasty. AJNR Am J Neuroradiol. 2009;30:496-9.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous vertebroplasty:Technical considerations. J Vasc Interv Radiol. 2003;14:953-60.
- [Google Scholar]
- Technical strategies and anatomic considerations for parapedicular access to thoracic and lumbar vertebral bodies. Skeletal Radiol. 2007;36:47-52.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous vertebroplasty for single osteoporotic vertebral body compression fracture:Results of unilateral 3-D percutaneous puncture technique. Indian J Orthop. 2015;49:245-50.
- [CrossRef] [Google Scholar]
- Percutaneous vertebroplasty for osteolytic metastases and myeloma:Effects of the percentage of lesion filling and the leakage of methyl methacrylate at clinical follow-up. Radiology. 1996;200:525-30.
- [Google Scholar]
- The effect of vertebral body percentage fill on mechanical behavior during percutaneous vertebroplasty. Spine (Phila Pa 1976). 2003;28:1549-54.
- [CrossRef] [PubMed] [Google Scholar]
- The biomechanics of vertebroplasty. The effect of cement volume on mechanical behavior. Spine (Phila Pa 1976). 2001;26:1537-41.
- [Google Scholar]
- Arandomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009;361:569-79.
- [Google Scholar]
- Arandomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009;361:557-68.
- [CrossRef] [PubMed] [Google Scholar]
- Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II):An open-label randomised trial. Lancet. 2010;376:1085-92.
- [Google Scholar]
- Is vertebroplasty a risk factor for subsequent vertebral fracture, meta-analysis of published evidence? Osteoporos Int. 2015;26:113-22.
- [Google Scholar]
- Percutaneous vertebroplasty for osteoporotic vertebral compression fracture. Cochrane Database Syst Rev. 2018;4:CD006349.
- [Google Scholar]
- Management of pulmonary cement embolism after percutaneous vertebroplasty and kyphoplasty:A systematic review of the literature. Eur Spine J. 2009;18:1257-65.
- [CrossRef] [PubMed] [Google Scholar]
- Pulmonary embolism caused by acrylic cement:A rare complication of percutaneous vertebroplasty. AJNR Am J Neuroradiol. 1999;20:375-7.
- [CrossRef] [Google Scholar]
- Percutaneous vertebroplasty and pulmonary cement embolism:Results from VERTOS II. AJNR Am J Neuroradiol. 2010;31:1451-3.
- [CrossRef] [PubMed] [Google Scholar]
- Dose-dependent epidural leakage of polymethylmethacrylate after percutaneous vertebroplasty in patients with osteoporotic vertebral compression fractures. J Neurosurg. 2002;96:56-61.
- [CrossRef] [Google Scholar]
- Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR):A multicentre, randomised, double-blind, placebo-controlled trial. Lancet. 2016;388:1408-16.
- [CrossRef] [Google Scholar]
- Is there a dose-response relationship of cement volume with cement leakage and pain relief after vertebroplasty? Dose Response. 2016;14:1559325816682867.
- [Google Scholar]
- The volumetric analysis of cement in vertebroplasty:Relationship with clinical outcome and complications. Spine (Phila Pa 1976). 2011;36:E761-72.
- [CrossRef] [PubMed] [Google Scholar]







