Translate this page into:
Fogarty-assisted flow redirection during conventional transarterial chemoembolization for caudate lobe hepatocellular carcinoma

*Corresponding author: Husameddin El Khudari, Department of Interventional Radiology, University of Alabama at Birmingham, Birmingham, Alabama, United States. helkhudari@uabmc.edu
-
Received: ,
Accepted: ,
How to cite this article: Ceballos D, Tine A, Varma R, El Khudari H. Fogarty-assisted flow redirection during conventional transarterial chemoembolization for caudate lobe hepatocellular carcinoma. Am J Interv Radiol 2022;6:1.
Abstract
Hepatocellular carcinoma (HCC) is the most common primary liver malignancy. Approximately 8% of patients with HCC are not suitable candidates for curative options. Caudate lobe HCC presents technical challenges for interventional radiologists. Caudate lobe HCC has higher local recurrence and poorer survival rate than other segments. Transarterial treatments of caudate HCC are difficult due to extreme variation of arterial supply. We present a case of a caudate lobe HCC with supply from the proper hepatic artery, which underwent successful conventional transcatheter arterial chemoembolization (cTACE) by utilizing a Fogarty catheter to direct the embolic material. The patient presented 5 days following the procedure with duodenitis and pancreatitis, which were managed conservatively. Follow-up imaging at 1 month showed significant improvement of the ischemic duodenitis/pancreatitis with successful cTACE.
Keywords
Transarterial chemoembolization
Hepatocellular carcinoma
Fogarty catheter
INTRODUCTION
Hepatocellular carcinoma (HCC) is the most common primary liver malignancy.[1] Approximately 8% of patients with HCC are not suitable candidates for curative options due to liver disease, malignancy, or comorbidities.[2] Interventional radiology procedures including percutaneous ablation (PA), radioembolization (TARE), and chemoembolization (TACE) have been widely adapted for the treatment of HCC. Caudate lobe/segment I HCC presents technical challenges for oncologic surgeons and interventional radiologists. In patients with caudate lobe HCC, the local recurrence and survival rate are worse than HCC located in other segments.[3] However, literature has demonstrated increased survival with TACE versus untreated HCC.[4] For interventional radiologists, each treatment modality has its own issues. With PA, the caudate lobe is located centrally and near hepatic vascular and biliary structures. This creates difficulty with ensuring the safety of adjacent structures and achieving adequate ablation. Transcatheter arterial treatments can vary in technique difficulty due to extreme variation of arterial supply.[3] Novel catheters have been utilized to assist with embolic delivery. They utilize an inflatable balloon to occlude the non-targeted vessel and minimize retrograde flow of embolic material. In rarer cases, occlusion of a distal vessel and delivery of embolic into a proximal branch are needed. We present a case of a caudate lobe HCC with supply from a branching vessel of the proper hepatic artery, which underwent successful conventional transcatheter arterial chemoembolization (cTACE) by utilizing a Fogarty catheter to direct the embolic material into the targeted branching vessel.
CASE REPORT
A 62-year-old male with a history of cirrhosis secondary to alcohol consumption and hepatitis C infection was referred from hepatology for the treatment of HCC. His surveillance magnetic resonance imaging (MRI) demonstrated recurrent multifocal HCC involving segment I (1.7 × 1.6 cm) and IVb (1.0 × 1.1 cm) [Figure 1]. Despite Milan criteria-based candidacy, the patient declined transplant or partial hepatectomies. Previously, the patient underwent drug-eluding beads transcatheter arterial chemoembolization for the treatment of segment III and V HCC. Imaging displayed no evidence of residual disease in the treated areas. Multidisciplinary tumor board recommendation was for cTACE. The patient was brought to the angiography suite (Philips Healthcare, Cambridge, MA, USA). Arterial access was obtained in the right common femoral artery. A 5 French RC-2 catheter (Cook Medical Inc., Bloomington, IN, USA) was used to perform a celiac angiogram which demonstrated two abnormal enhancements in the suspected liver segments.
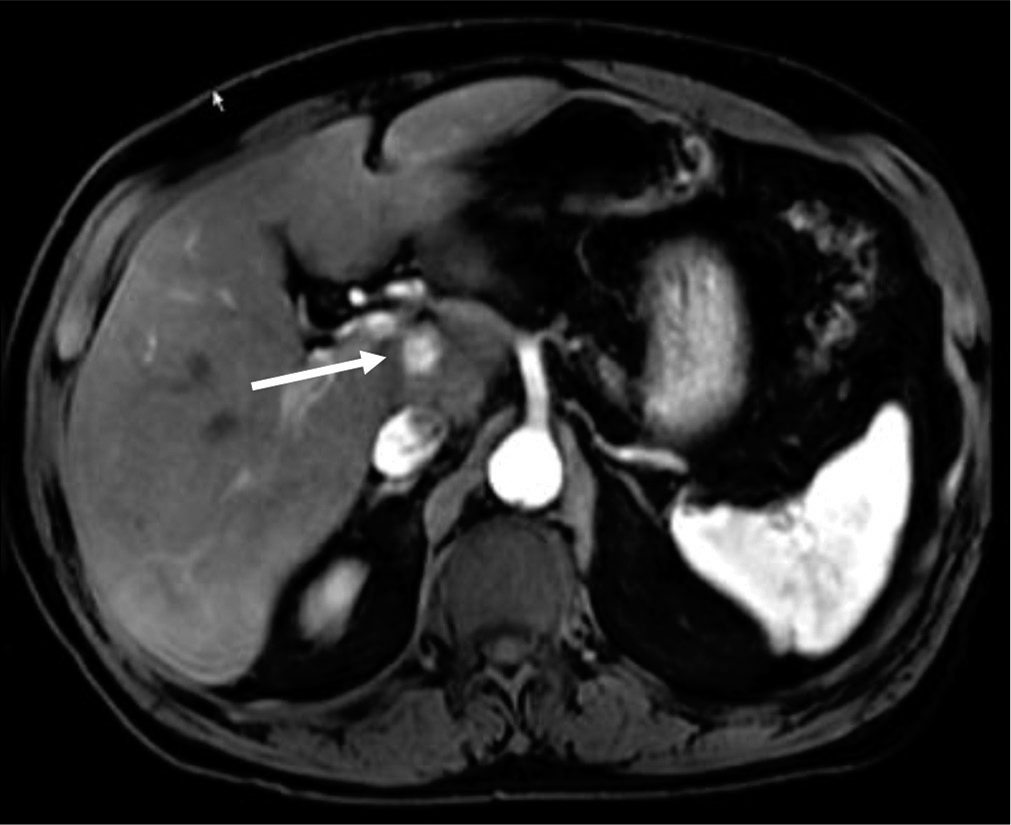
- A 62-year-old male with a history of cirrhosis secondary to alcohol consumption and hepatitis C infection was referred from hepatology for the treatment of hepatocellular carcinoma (HCC). T1 fat-saturated arterial phase liver magnetic resonance imaging demonstrating a small 1.7 cm rounded, enhancing HCC within caudate lobe (white arrow).
A 2.4 French Progreat microcatheter (Terumo Medical Corporation, Somerset, NJ, USA) was used to perform selective cTACE of the segment IVb lesion. The chemoembolic agent was compromised of 5 ml mixture of ethiodized oil (lipiodol), 50 mg doxorubicin, and 3 mL of Visipaque (GE Healthcare, Boston, MA) 320 mg. The segment IVb was treated until arterial flow stasis and early portal venous filling was identified. Then, attention was shifted to perform cTACE of the segment I HCC.
Delayed digital subtraction angiography of the proper hepatic artery demonstrated a branching vessel arising proximally from it, supplying the caudate lobe HCC [Figure 2a]. A cone-beam computerized tomography was performed to confirm the angiographic findings and caudate lobe enhancement corresponding to the pre-procedural MRI was seen [Figure 2b]. Microcatheters and wires were used to selectively catheterize the targeted vessel, however, without success due to small vessel size and tortuosity. Therefore, the vascular sheath was exchanged for a Cook 7 French Flexor Ansel 2 Guiding Sheath (Cook Medical Inc., Bloomington, IN, USA). Then, a 5.5 French Fogarty Thru-Lumen embolectomy catheter (Edwards Lifesciences, Irvine, CA, USA) was inserted into the distal proper hepatic artery and inflated at the bifurcation of the right and left hepatic arteries. No systemic heparin was administrated. The microcatheter was reinserted and its tip placed proximal to the Fogarty balloon. Contrast was injected confirming preferential flow into the tumor arterial branch without contrast flow into the right and left hepatic arteries. The administration was monitored with fluoroscopy to minimize non-target delivery. The Fogarty balloon was inflated in 2–3 min intervals and deflated to allow perfusion of liver for 2–3 min. Tumoral staining was observed during and after the delivery of embolic agents [Figure 3].

- (a) Delayed digital subtraction angiography of the proper hepatic artery demonstrating a tiny tortuous parasitized branching vessel (white arrow) from the proper hepatic artery supplying the caudate lobe hepatocellular carcinoma (HCC). (b) Intraprocedural cone-beam computerized tomography demonstrating focal enhancement consistent with the caudate lobe HCC (white arrow).

- Intraprocedural anterior-posterior radiograph demonstrating staining of the caudal lobe hepatocellular carcinoma and Fogarty balloon and microcatheter in situ (white arrow).
A digital subtraction angiogram from the proper hepatic artery was performed demonstrating patency of the proximal vasculature and stasis of flow within the treated vessels [Figure 4]. The catheters/sheaths were removed, and access was closed with Angio-Seal closure device (Terumo Medical Corporation, Somerset, NJ, USA). The patient was discharged home after recovery. The patient presented 5 days after procedure with clinical symptoms of acute duodenitis/pancreatitis and confirmed with computed tomography imaging [Figure 5]. The findings were suggestive of ischemic etiology, likely from non-targeted embolic reflux. In accordance with SIR adverse event classification, this would be considered a Class D complication due to prolonged hospitalization/unplanned increased level of care. The patient was managed conservatively for 3 days with hydration, pain control, and antibiotics. He was discharged home and follow-up MRI imaging at 4 weeks showed significant improvement of the ischemic duodenitis/pancreatitis with successful cTACE of both lesions [Figure 6a and b].

- Digital subtraction angiogram with catheter within the proper hepatic artery demonstrating no antegrade flow into the right or left hepatic artery, stasis of flow within the targeted vessel (white arrow), with tumoral lipiodol staining, and patency of the proximal vasculature, the gastroduodenal artery (black arrow).

- Computed tomography of abdomen and pelvis with intravenous contrast demonstrates diffuse thickening of the duodenum consistent with duodenitis. In addition, irregular enhancement, cystic changes, and peripancreatic inflammation were seen consistent with pancreatitis (white arrow).

- (a) T1 fat-saturated arterial phase liver magnetic resonance imaging (MRI) (3-month post-cTACE) demonstrating non-viable caudate lobe lesion with no recurrent or residual disease (white arrow). (b) T1 fat-saturated portal venous phase liver MRI (3-month post-cTACE) demonstrating normal pancreas and duodenum (white arrow).
DISCUSSION
The evolution of interventional techniques and equipment innovations is the cornerstone of interventional radiology. Many of these innovations are spurn from complex, technically challenging cases. TACE has been utilized for the treatment of caudate lobe HCC but can be technically difficult for interventional radiologists.[5] The reported technical success rate for selective caudate lobe TACE is 71% with local recurrence at 77%.[6] The difficulties with both interventional and surgical treatments for caudate disease lead to its poor prognosis.[5] While proximal occluding catheters are commonly used to perform embolization in TACE and TARE, the utilization of distal occlusion for proximal delivery is rare[7] However, in caudate HCC disease, arterial supply has a propensity for complex origins. For example, Yoon et al. reported two direct proper hepatic arteries supply in 175 caudate lobe HCC cases.[8] Therefore, proximal occlusion balloon would not suffice. Pasciak et al. have demonstrated technical ability with a double balloon microcatheter involving four cases of HCC with small target artery arising from the parent artery.[7] Despite success, the double balloon catheter is not readily available in the United States.
CONCLUSION
This case demonstrates the usage of common equipment within interventional radiology departments achieving chemoembolic delivery for caudate lobe HCC disease. The patient did develop acute duodenitis and pancreatitis from likely chemoembolic reflux in the gastroduodenal artery (GDA). However, the patient required only conservative medical therapy for full recovery. At 1 month, follow-up imaging demonstrated successful cTACE of the caudate lobe lesion. Retrospectively, prophylactic embolization of the GDA would have decreased the likelihood of this complication occurring. Despite this, we were able to perform successful cTACE of this lesion without residual or recurrent disease in the caudate lobe at 1 month.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Cancer of the Liver and Intrahepatic Bile Duct-cancer Stat Facts SEER. 2021. Available from: https://www.seer.cancer.gov/statfacts/html/livibd.html [Last accessed on 2021 Jun 14]
- [Google Scholar]
- Percutaneous ablation of hepatocellular carcinoma: Current status. J Vasc Int Radiol. 2010;21:S204-13.
- [CrossRef] [PubMed] [Google Scholar]
- Subsegmental transcatheter arterial embolization for hepatocellular carcinoma in the caudate lobe. J Vasc Int Radiol. 1998;9:501-8.
- [CrossRef] [Google Scholar]
- Segmental transcatheter arterial chemoembolization treatment in patients with cirrhosis and inoperable hepatocellular carcinomas. J Vasc Interv Radiol. 2002;13:995-9.
- [CrossRef] [Google Scholar]
- A case of hepatocellular carcinoma in the caudate lobe successfully treated by transcatheter arterial chemoembolization using drug-eluting beads. Korean J Hepatol. 2010;16:405-9.
- [CrossRef] [PubMed] [Google Scholar]
- Use of proximal side-holemicro-balloon catheter in transcatheter hepatic arterial chemoembolization. Minim Invasive Ther Allied Technol. 2017;26:372-6.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of an antireflux catheter on target volume particulate distribution in liver-directed embolotherapy: A pilot study. J Vasc Interv Radiol. 2015;26:660-9.
- [CrossRef] [PubMed] [Google Scholar]
- Hepatocellular carcinoma in the caudate lobe of the liver: Angiographic analysis of tumor-feeding arteries according to subsegmental location. J Vasc Interv Radiol. 2008;19:1543-50. quiz 1550
- [CrossRef] [PubMed] [Google Scholar]







