Translate this page into:
Percutaneous pulmonary thrombectomy in hemodynamically unstable pediatric patient

*Corresponding author: Brian James Montague, Department of Interventional Radiology, SDI Diagnostic and Interventional Radiology at St. Joseph Hospital, 4516 N Armenia Avenue, Tampa -33510, Florida, United States.bjmontague74@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Montague BJ. Percutaneous pulmonary thrombectomy in hemodynamically unstable pediatric patient. Am J Interv Radiol 2020;4:13.
Abstract
An 11-year-old girl was referred to interventional radiology with a suspected pulmonary embolism (PE) 10 days post-resection of a benign craniopharyngioma. Acute massive PE was confirmed through computed tomography (CT) with extensive thrombus burden and CT evidence of high-grade right ventricular strain. Due to profound hypoxemia and hemodynamic instability, the patient was placed on extracorporeal membrane oxygenation and emergency percutaneous mechanical thrombectomy through the FlowTriever® System (Inari Medical, Irvine, CA) was pursued. A large volume of thrombus was extracted through aspiration without the need for thrombolytics. Postprocedure pulmonary angiography confirmed complete restoration of blood flow to both lungs and resolution of pulmonary symptoms continues 9 months after the procedure.
Keywords
Pulmonary embolism
Percutaneous thrombectomy
Pediatric
INTRODUCTION
Venous thromboembolism (VTE) is a common risk for patients undergoing neurosurgery for several reasons, including the long duration of procedures, reduced mobility during recovery, and the direct release of pro-coagulants from brain tissue.[1,2] Patients undergoing surgery to remove brain tumors are particularly susceptible to VTE events, regardless of proactive thromboprophylaxis.[3-6] The treatment of VTE following major surgery is complicated by the contraindication of common treatments for VTE, such as thrombolytics, due to the associated bleeding risks.[7] We report a case of a pediatric patient presenting with acute massive pulmonary embolism (PE) following neurosurgery, in which emergency percutaneous mechanical thrombectomy through large-bore aspiration with the FlowTriever® System (Inari Medical, Irvine, CA) was utilized to safely and effectively extract thrombus and restore normal hemodynamics without the need for thrombolytics.
CASE REPORT
An 11-year-old girl was referred to interventional radiology with a suspected PE. Ten days prior, she had undergone surgery to remove a benign craniopharyngioma. While in rehabilitation, she became tachypneic with a respiratory rate of 28 breaths/min and an oxygen saturation of 91% on room air. She experienced a transient hypotensive state, with a systemic blood pressure of 80/54 mmHg and an elevated heart rate as high as 120 bpm, before becoming normotensive. Her troponin levels were elevated at 0.95 ng/mL. Acute PE was confirmed through computed tomography (CT) with extensive thrombus burden primarily affecting the right main pulmonary artery (PA) and evidence of high-grade right ventricular (RV) strain [Figure 1]. After the CT scan, the patient remained stable, so she was admitted to the pediatric intensive care unit for observation and started on heparin. Approximately 2 h later, she developed acute respiratory failure with severe hypoxemia and shock, with a blood pressure of 62/40 mmHg and a heart rate of 140 bpm. The patient was intubated and placed on extracorporeal membrane oxygenation (ECMO). She was subsequently brought to interventional radiology for emergency percutaneous mechanical thrombectomy through the FlowTriever System.
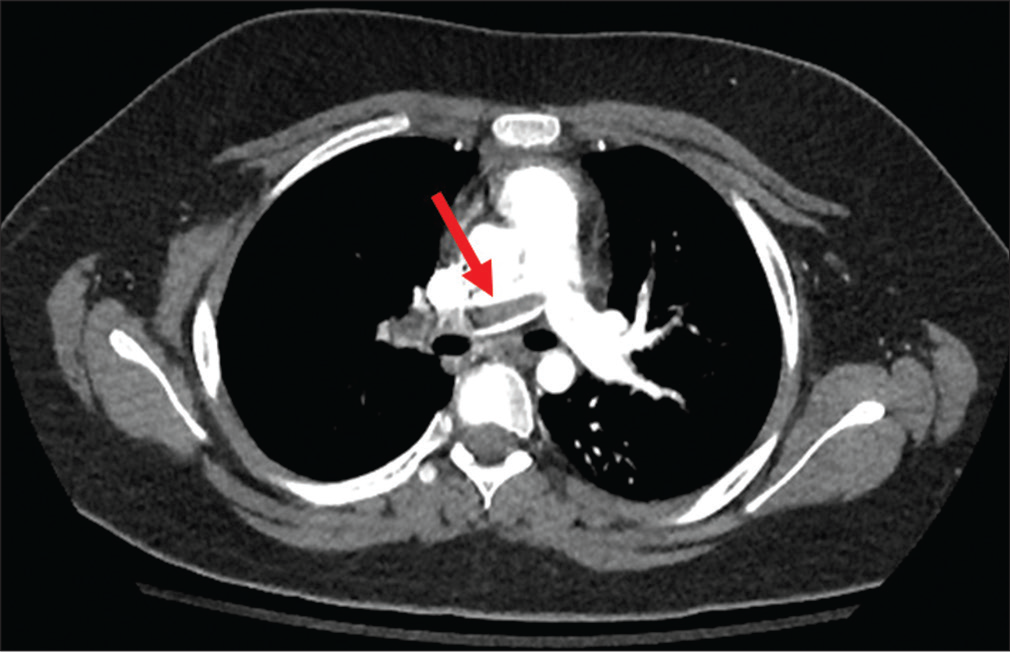
- An 11-year-old girl who presented with a hemodynamically unstable pulmonary embolism. Computed tomography shows extensive thrombus burden primarily affecting the right pulmonary artery (red arrow).
Heparin was continued throughout the procedure. Ultrasound-guided venous access was pursued below the inguinal ligament to reduce the risk of retroperitoneal hemorrhage. Right common femoral vein access was achieved through a 22-F introducer with careful dilation of the vessel, after performing a venogram to evaluate iliac vein caliber and patency. An angled pigtail catheter was used to traverse the right heart and gain access to the main PA. Pulmonary angiography confirmed extensive thrombus burden, with lung perfusion only present in the left upper lobe [Figure 2]. The 20-F FlowTriever aspiration guide catheter (Triever20) was tracked over the wire into the right main PA [Figure 3]. A volume-controlled aspiration through a 60 cc large-bore syringe was performed in the right main PA which extracted a small amount of chronic thrombus. We then introduced a medium FlowTriever catheter, consisting of three nitinol mesh disks, through the Triever20 to dislodge the thrombus, followed by another aspiration which extracted more thrombus. The third aspiration following the use of the FlowTriever disks yielded extensive acute and chronic thrombus from the right main PA, restoring perfusion of the right lung. Two additional aspirations in the left PA extracted further thrombus and restored perfusion of the left lower lobe [Figures 4 and 5]. Of note, a thrombus cast of the majority of the right pulmonary arterial tree was removed en bloc.

- An 11-year-old girl who presented with a hemodynamically unstable pulmonary embolism. Pulmonary angiography performed through a pigtail catheter demonstrates pulmonary perfusion only present in the left upper lobe, with no perfusion in the left lower lobe or right lung (red arrows).

- An 11-year-old girl who presented with a hemodynamically unstable pulmonary embolism. The FlowTriever aspiration guide catheter (Triever20) tracked over the wire through the right heart and into the main PA for mechanical thrombectomy.

- An 11-year-old girl who presented with a hemodynamically unstable pulmonary embolism. Extensive thrombus extracted from the right and left pulmonary arteries via percutaneous thrombectomy without the need for thrombolytics.

- An 11-year-old girl who presented with a hemodynamically unstable pulmonary embolism. Post-thrombectomy, pulmonary angiography reveals restored perfusion to both the right and left lungs.
Following thrombectomy, the patient had immediate improvement in oxygen saturation (100%), heart rate (102 bpm), and blood pressure (102/62 mmHg). She experienced no access site complications despite the large-bore introducer. The patient was extubated and ECMO was discontinued later that day. Troponin levels normalized within 24 h and the patient was asymptomatic from a respiratory standpoint two days following the procedure. She continued to improve with inpatient physical therapy and was discharged 1 week later.
The patient was seen in follow-up 9 months after the procedure and had persistent resolution of pulmonary symptoms. There were no signs of the right heart strain through CTA and her oxygen saturation was 100% on room air.
DISCUSSION
We successfully treated acute massive PE in a pediatric patient, who had recently undergone surgery to remove a benign craniopharyngioma, through percutaneous thrombectomy without the need for thrombolytics. We extracted a large volume of thrombus from the right and left main PAs and restored perfusion in both lungs.
Treating massive PE in a patient recovering from major surgery is challenging, as an aggressive treatment approach to restore hemodynamic stability must be balanced against the increased bleeding risk. Thrombolytics, a common treatment option for massive PE, is contraindicated in patients who underwent major surgery within the prior 3 weeks.[7] Even in patients without contraindications, thrombolytics increase the risk of bleeding as compared to anticoagulation, with a meta-analysis estimating a 9.24% major bleeding rate and a 1.46% intracranial hemorrhage rate with thrombolytic therapy.[8]
Further complicating this case was the age of the patient, as there are little available data or case reports of large-bore mechanical pulmonary thrombectomy being performed in a pediatric setting. The large-bore Triever20 catheter tracked smoothly through the right heart of this patient and into the main PAs for treatment. In addition, the use of the large 22-F sheath did not cause access site injury in this pediatric patient after careful dilation of the vessel.
Massive PE can cause the right heart to quickly spiral to failure, as the presence of PA thrombus increases the RV pressure and causes it to dilate, subsequently affecting left ventricle filling and further exacerbating the cardiac dysfunction.[9]An additional benefit of mechanical thrombectomy is the immediate unloading of the RV, stopping the cycle from perpetuating. Following thrombus extraction, the patient had immediate on-table improvements in hemodynamics, including oxygen saturation, heart rate, and blood pressure.
CONCLUSION
Despite the challenges associated with treating an acute massive PE in a pediatric patient who had recently undergone major surgery, we safely and effectively used percutaneous mechanical thrombectomy with the FlowTriever system to extract a large volume of thrombus while avoiding the significant bleeding risk associated with thrombolytics. The patient experienced immediate on-table hemodynamic improvement and has persistent resolution of pulmonary symptoms at 9-month follow-up.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The risk of venous thromboembolism is increased throughout the course of malignant glioma: An evidence-based review. Cancer. 2000;89:640-6.
- [CrossRef] [Google Scholar]
- Epidemiology of venous thromboembolism in 9489 patients with malignant glioma. J Neurosurg. 2007;106:601-8.
- [CrossRef] [PubMed] [Google Scholar]
- Increased risk of venous thromboembolism in patients with brain tumors: A systematic review and meta-analysis. Thromb Res. 2016;137:58-63.
- [CrossRef] [PubMed] [Google Scholar]
- The incidence of postoperative thromboembolic complications following surgical resection of intracranial meningioma. A retrospective study of a large single center patient cohort. Clin Neurol Neurosurg. 2014;123:150-4.
- [CrossRef] [PubMed] [Google Scholar]
- Development of venous thromboembolism (VTE) in patients undergoing surgery for brain tumors: Results from a single center over a 10 year period. J Clin Neurosci. 2015;22:519-25.
- [CrossRef] [PubMed] [Google Scholar]
- Deep venous thrombosis and pulmonary embolisms in adult patients undergoing craniotomy for brain tumors. Neurol Res. 2013;35:206-11.
- [CrossRef] [PubMed] [Google Scholar]
- 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European respiratory society (ERS): The task force for the diagnosis and management of acute pulmonary embolism of the European society of cardiology (ESC) Eur Respir J. 2019;54:1901647.
- [CrossRef] [PubMed] [Google Scholar]
- Thrombolysis for pulmonary embolism and risk of all-cause mortality, major bleeding, and intracranial hemorrhage: A meta-analysis. JAMA. 2014;311:2414-21.
- [CrossRef] [PubMed] [Google Scholar]
- Role of interventional radiologist in the management of acute pulmonary embolism. Semin Intervent Radiol. 2020;37:62-73.
- [CrossRef] [PubMed] [Google Scholar]






