Translate this page into:
CT-guided percutaneous lung biopsy: Correlation between diagnostic yield, lung lesion size, and lobar distribution

*Corresponding author: Adib R. Karam, MD, Department of Radiology, Alpert Medical School of Brown University, Providence, Rhode Island, United States. karamadib@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Wilson M, Karam AR, Baird GL, Furman MS, Grand DJ. CT-guided percutaneous lung biopsy: Correlation between diagnostic yield, lung lesion size, and lobar distribution. Am J Interv Radiol 2021;5:14.
Abstract
Objectives:
The aim of this retrospective study was to investigate the relationship between lung lesion lobar distribution, lesion size, and lung biopsy diagnostic yield.
Material and Methods:
This retrospective study was performed between January 1, 2013, and April 30, 2019, on CT-guided percutaneous transthoracic needle biopsies of 1522 lung lesions, median size 3.65 cm (range: 0.5– 15.5 cm). Lung lesions were localized as follows: upper lobes, right middle lobe and lingual, lower lobes superior segments, and lower lobes basal segments. Biopsies were classified as either diagnostic or non-diagnostic based on final cytology and/or pathology reports. Results were considered diagnostic if malignancy or a specific benign diagnosis was established, whereas atypical cells, non-specific benignity, or insufficient specimen were considered non-diagnostic.
Results:
The positive predictive value (PPV) of a diagnostic yield was 85%, regardless of lobar distribution. Because all PPVs were relatively high across locations (84–87%), we failed to find statistically significant difference in PPV between locations (P = 0.79). Furthermore, for every 1 cm increase in target size, the odds of a diagnostic yield increased by 1.42-fold or 42% above 85%. Although target size increased the diagnostic yield differently by location (between 1.4- and 1.8-fold across locations), these differences failed to be statistically significant, P = 0.55.
Conclusion:
Percutaneous transthoracic needle biopsy of lung lesions achieved high diagnostic yield (PPV: 84– 87%) across all lobes. A 42% odds increase in yield was achieved for every 1 cm increase in target size. However, this increase in size failed to be statistically significant between lobes.
Keywords
Biopsy
CT
Lung biopsy
Lung cancer
Lung nodule
INTRODUCTION
The leading cause of cancer-related death is lung cancer.[1] Early detection of lung cancer with CT imaging has been proven to reduce lung cancer-related mortality for high-risk patient populations.[1,2] Accordingly, lung cancer screening has become a standardized guideline by the United States Preventive Services Task Force.[3] Due to widespread availability of CT imaging and increased CT screening for lung cancer, more pulmonary nodules are being detected which often ultimately require biopsy and histopathologic confirmation for a definitive diagnosis.[4]
Percutaneous transthoracic needle biopsy (PTNB) of lung lesions is highly efficacious, offering 90% sensitivity and 95% specificity;[5,6] however, the potential of non-diagnostic results is still burdensome. Improving the diagnostic yield of PTNB would lower the costs associated with repeat biopsies, decrease time until diagnosis is established, and reduce patient stress.
There are several factors associated with a reduced diagnostic yield of PTNB, including smaller lesion size, parenchymal hemorrhage, and use of fine-needle aspiration alone (without core needle biopsy), and biopsy of nodules with ground-glass consistency on CT imaging.[5,7] Investigators demonstrated that among nodules smaller than 1 cm, lobar distribution of nodules impacted diagnostic performance.[8] In this retrospective study, we sought to evaluate whether (1) diagnostic yield varied when lung lesions were stratified by location and (2) whether the trend of increased diagnostic performance with increased lesion size differed depending on their lobar distribution. Specifically, because respiratory motion affects lower lobe lesions to a greater extent than upper lobe lesions, we hypothesized that yield would be higher for lesions in the upper lobes and superior segments of the lower lobes relative to nodules in the right middle lobe, lingula and basal segments of the lower lobes. In addition, we hypothesized that yield would increase as lesion size increased, especially for lesions in the middle lobe, lingula, and basal segments of the lower lobes relative to lesions in the superior segments of the lower lobes and upper lobes.
MATERIAL AND METHODS
This multi-center retrospective study was HIPAA-compliant and received institutional review board approval. Informed consent was waived due to the retrospective nature of the study.
Study sample
Between January 1, 2013, and April 30, 2019, a total of 1522 CT-guided PTNBs were performed at two different sites within one academic medical center. Included lung lesions measured between 0.5 and 15.5 cm, median size = 3.65 cm.
Biopsy procedure and histopathological findings
Patients with prior CT imaging were referred for PTNB by pulmonologists, thoracic surgeons, or medical oncologists. Biopsies were performed under CT-fluoroscopy (Optima CT580 W, GE Healthcare, Chicago, IL, USA and Toshiba, Aquilion 16, Toshiba Medical Systems, Tokyo, Japan) by one of 12 subspecialized radiologists, each of whom had performed at least 50 PTNBs prior to January 1, 2013. All patients received local anesthesia, and some received moderate sedation. All biopsies were performed using coaxial technique and a fine-needle aspiration and core biopsy was obtained. Biopsy specimens were fixed and histologically assessed as diagnostic (malignant or specific benign diagnosis) or non-diagnostic (insufficient specimen, atypical cells, or non-specific benign diagnosis) based on final cytology and or pathology reports. Non-diagnostic results were further evaluated with repeat imaging and/or biopsy for definitive diagnostic classification.
Data analysis
Images stored in a Picture Archiving and Communication System on a clinical workstation were used to analyze nodule maximum dimensions on the lung window setting. Lung segments were assigned to each nodule based on both the procedural CT images and the original, multiplanar CT. Lung lesions were localized as follows: upper lobes (UL), middle lobe and lingula (ML), lower lobes superior segments (LLS), and lower lobes basal segments (LLB).
Statistics
All analyses were conducted using SAS Software 9.4 (SAS Inc., Cary, NC) with the GLIMMIX procedure. All modeling was accomplished using generalized linear mixed modeling assuming a binomial distribution with sandwich estimation where observations were nested within patients; this was done to prevent violation of independence. Both main (lobe location and nodule size) and interaction effects (lobe location by size) were evaluated, and point estimates were converted to odds ratios with 95% confidence intervals.
RESULTS
During the study period, a total of 1397 patients with 1522 PTNBs were included in the study. Lesions measured between 0.5 and 15.5 cm, median nodule size = 3.65 cm. Of the 1522 observations, 692 were male and 830 were female. The age range was 19–90 years, median age = 70 years.
The positive predictive value (PPV) of a diagnostic yield was 85% across all lobes. In the LLB and ML, the PPV was 86%; in the UL, the PPV was 84%, and in the LLS, the PPV was 87% [Table 1]. There was no statistically significant difference in PPV between these locations (P = 0.79). For every 1 cm increase in size of target lesion, the odds of a diagnostic yield increased by 1.42-fold or 42% above 85% (P < 0.0001) [Figure 1]. Although the increased target size affected the diagnostic yield differently according to the lobar location (1.5-fold in the LLB, 1.8-fold in the LLS, 1.4-fold in the ML, and 1.4-fold in the UL), these differences failed to be statistically significant (P = 0.55).
| Location | PPV | 95% CI | P-value |
|---|---|---|---|
| LLB | 85.7% | 82.1–88.7 | 0.7866 |
| LLS | 87.1% | 80.9–91.5 | |
| ML | 85.8% | 80.0–90.2 | |
| UL | 84.3% | 81.3–86.9 | |
| All | 85.2% | 83.3–86.9 | |
| Location by size | Odds ratio | 95% CI | P-value |
| LLB | 1.497 | 1.154–1.943 | 0.5508 |
| LLS | 1.833 | 1.269–2.648 | |
| ML | 1.444 | 1.019–2.046 | |
| UL | 1.356 | 1.117–1.647 | |
| All | 1.417 | 1.232–1.629 | <0.0001 |
PPV: Positive predictive value, LLB: Lower lobes, basal segments, LLS: Lower lobes, superior segments, ML: Right middle lobe and lingula, UL: Upper lobes.
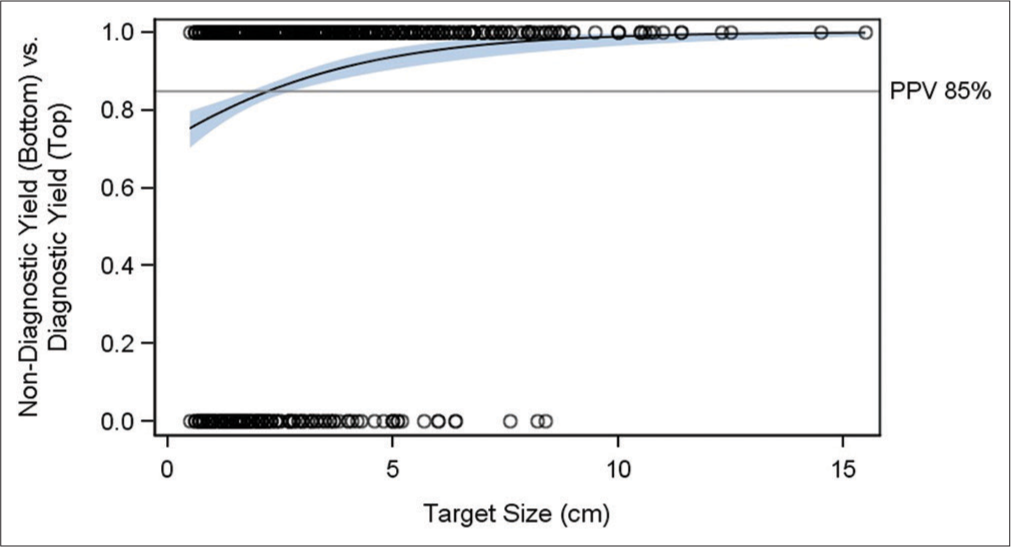
- Relationship between Target Size and Positive Yield. Y-axis is the likelihood of diagnostic yield between 0% and 100%. X-axis is the target size between 0 cm and 16 cm. Black circles are the actual data points where yield was diagnostic (top) or non-diagnostic (bottom). Grey horizontal line represents the 85% positive predictive value of diagnostic yield. Black line represents the positive predictive value of positive yield regardless of target size. Blue line represents the odds increase (slope) in positive yield as target yield increases above the PPV. Light blue band represents the 95% confidence band.
DISCUSSION
PTNB is highly accurate for diagnosing pulmonary lesions identified on CT imaging;[5] however, results can be non-diagnostic in as many as 27.6% of biopsies, including up to 40% of nodules <1 cm in size.[9] Non-diagnostic results, which can be categorized as either atypical cells, non-specific benign diagnosis, or inadequate specimen, pose a frustration to patients and increase risk of complications as well as cost of care by necessitating repeat biopsy and/or imaging.[10] Understanding factors that impact diagnostic yield of PTNB is important in the management of patients requiring definitive diagnosis of lung lesions.
Factors that influence diagnostic yield include lesion size, parenchymal hemorrhage, type of biopsy, and nodule consistency.[5,7] Most prominently, increasing lesion size portends a higher likelihood of diagnostic success. In our study, we sought to evaluate (1) whether this trend differed by lobar distribution of pulmonary nodules and (2) whether diagnostic yield differed for nodules regardless of size when stratified by lobar distribution. Investigators showed that among nodules smaller than 1 cm, diagnostic yield varied depending on lobar location, likely due to factors such as differential diaphragmatic excursion during respiration.[8] Here, we show this trend does not impact nodules when analyzed independent of size. In our study, the PPV was equally high across all lung lobes, roughly 85%. This is possibly due to a “ceiling effect.” The odds of a diagnostic yield increased by 1.42-fold for every 1 cm increase in size above 85% PPV, corroborating prior literature.[5] Although this trend was still present, it was not significantly different when the data were stratified by lobar region.
Our study is limited by its retrospective nature. Another limitation is the lack of standardized biopsy technique including the number of passes during each biopsy and the use of fine needle aspiration and core biopsy which accurately reflects our current practice, and the fact that some patients required moderate sedation before biopsy.
CONCLUSION
The diagnostic performance of PTNB of lung lesions is not impacted by lobar distribution. We found that increasing lesion size was a strong predictor of increased diagnostic yield; however, this trend was not significantly different when stratified by lobar location. When planning a PTNB, it is more important for the clinician to consider other factors affecting diagnostic yield, such as lesion size and consistency, as well as factors affecting complication rate, such as lesion depth, needle choice, and presence of emphysema rather than lobar location.[11,12]
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The national lung screening trial: Overview and study design. Radiology. 2011;258:243-53.
- [CrossRef] [Google Scholar]
- Screening for Lung Cancer: Systematic Review to Update the U.S. Preventive Services Task Force Recommendation Rockville, MD: Agency for Healthcare Research and Quality; 2013.
- [Google Scholar]
- Recent trends in the identification of incidental pulmonary nodules. Am J Respir Crit Care Med. 2015;192:1208-14.
- [CrossRef] [Google Scholar]
- CT-guided percutaneous core needle biopsy of pulmonary nodules smaller than 2 cm: Technical aspects and factors influencing accuracy. J Bras Pneumol. 2018;44:307-14.
- [CrossRef] [Google Scholar]
- British thoracic society guidelines for the investigation and management of pulmonary nodules. Thorax. 2015;70(Suppl 2):ii1-54.
- [Google Scholar]
- Percutaneous CT-guided aspiration and core biopsy of pulmonary nodules smaller than 1 cm: Analysis of outcomes of 305 procedures from a tertiary referral center. AJR Am J Roentgenol. 2013;201:964-70.
- [CrossRef] [Google Scholar]
- CT-guided biopsy of pulmonary nodules =10 mm: Diagnostic yield based on nodules' lobar and segmental distribution. Clin Imaging. 2020;66:7-9.
- [CrossRef] [Google Scholar]
- Nondiagnostic percutaneous transthoracic needle biopsy of lung lesions: A multicenter study of malignancy risk. Radiology. 2019;290:814-23.
- [CrossRef] [Google Scholar]
- Clinical significance of non-diagnostic pathology results from percutaneous transthoracic needle lung biopsy: Experience of a tertiary hospital without an on-site cytopathologist. Respirology. 2009;14:1042-50.
- [CrossRef] [Google Scholar]
- Complication rates of CT-guided transthoracic lung biopsy: Meta-analysis. Eur Radiol. 2017;27:138-48.
- [CrossRef] [Google Scholar]






