Translate this page into:
Causes and Treatment of Bile Leaks at the Puncture Site After Percutaneous Transhepatic Biliary Decompression

*Corresponding author: Dr. Nasir Babakhan Kondori, Radiology Consultant and Interventional Fellow, SUMS (Shiraz University of Medical Sciences), Radiology Department, Namazi Hospital, Namazi Square, Shiraz, Iran. nasirbabakhan@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rasekhi A, Kondori NB. Causes and Treatment of Bile Leakage at the Puncture Site Following Percutaneous Transhepatic Biliary Decompression. Am J Interv Radiol 2019;3:8.
Abstract
Introduction:
Bile leaks at the puncture site after percutaneous transhepatic biliary decompression (PTBD) are not uncommon and cause a lot of problems for patients with non-resectable biliary malignant obstruction. However, to the best of the authors’ knowledge, no study is conducted to establish the causes and to find an appropriate treatment. The current study was conducted on 264 patients who underwent PTBD for a malignant biliary obstruction.
Material and Methods:
This retrospective study reviewed 264 patients with non-resectable malignant biliary obstruction requiring PTBD. A two-stage biliary decompression is done. An 8Fr pigtail catheter is placed for PTBD, the patients would return after two days for stent placement. After stent placement, an 8 Fr pigtail catheter (internal – external) would be placed for flushing, and also for cholangiography. The patients are then observed for another two days. Patients who have persistent puncture site bile leakage after 24 hours are considered to have a bile leak. In these patients, cholangiography is performed. If cholangiography reveals stent occlusion, stent reopening by irrigation/ballooning is done. For those with patent stents and bile leakage, an internal-external biliary drain is placed which does not solve the problem, and a cholangiography is done into the drain tract via a syringe.
Results:
Sixteen of 264 patients who underwent percutaneous biliary decompression developed bile leakage at the puncture site. Twelve of these patients demonstrated an occluded biliary stent and their bile leak resolved after irrigation/ballooning. Four patients with bile leak demonstrated patent biliary stents and persistent leakage despite internal-external biliary drain placement. Cholangiograms in these patients demonstrated connections from the stented biliary system (the ipsilateral system), branches of a different occluded biliary system (the contralateral biliary tract), and the drain tract. All four patients underwent PTBD of the contralateral biliary system with subsequent resolution of their bile leak.
Discussion:
One of the complications of PTBD is bile leakage at the puncture site which could have two reasons. The most common is stent occlusion by clot and debris which can be managed by irrigation/ stenting. The second mechanism of bile leakage, not reported previously, was a fistulous connection between the drained biliary system (the ipsilateral system) and a separate obstructed biliary system (the contralateral system).
We would like to refer to this mechanism of bile leak “Yo-Yo reflux” for its specific pattern of cholangiography. The Yo-Yo reflux mechanism of bile leaks occurs when a small branch from the adjacent separated contralateral system is transgressed inadvertently during ipsilateral biliary drainage. High-pressure bile fluid from the obstructed system flows through the lower pressure ipsilateral system and through the cannulation tract and onto the skin surface. In the Yo-Yo mechanism, stenting of the contralateral side is the only treatment.
Conclusion:
Bile leakage at the puncture site after PTBD has two major causes. The most common is stent occlusion by clot/debris which is diagnosed by cholangiography and treated by irrigation/ballooning. The second cause is Yo-Yo reflux which is diagnosed by cholangiography injecting directly into the orifice of skin fistula and treated by contralateral stenting.
Keywords
Bile leak
Biliary intervention
Biliary stenting
Biliary complications
Percutaneous transhepatic biliary drainage
INTRODUCTION
Biliary obstruction has a multitude of causes including malignancies such as cholangiocarcinoma, gallbladder carcinoma, pancreatic adenocarcinoma, and metastases. Unfortunately, many of these cases are non-resectable at the time of diagnosis. Contraindications to surgical resection vary by malignancy. But in general, extrahepatic extension, liver metastasis, involvement of the main portal vein, bilateral portal vein branches, second-order biliary branches, superior mesenteric artery, hepatic artery, and lymph nodes of the pancreatic/celiac axis.[1]
Biliary drainage is indicated for cholangitis, jaundice-associated pruritus, hyperbilirubinemia, and severe pain secondary to biliary obstruction. This may be performed via endoscopic retrograde cholangiopancreatography (ERCP) or percutaneously. Patients with single central lesions benefi t the most from ERCP. However, ERCP is a technically difficult procedure, and many patients have contraindication to the procedure such as coagulopathies, bowel perforation, or alternate anatomy (i.e., Roux-en-Y).[2]
Percutaneous transhepatic biliary drainage (PTBD) is an alternative procedure which may benefi t patients with a contraindication to ERCP or patients with peripheral obstructions.[3] Biliary stasis from obstruction leads to hepatic necrosis and atrophy. If greater than 50% of the liver is obstructed, the patient will eventually develop liver failure without drainage. Atrophic lobes or segments and lobes with portal vein thrombus should not be drained as liver function of the aff ected region is unlikely to improve.[2]
A unique consequence of peripheral lesions is biliary separation [Figure 1] in which a tumor at a branch point separates biliary drainage from diff erent hepatic lobes or segments. While attempting to drain a specifi c bile duct segment (hereinafter referred to as the ipsilateral system), a diff erent adjacent segment bile duct (hereinafter referred to as the contralateral system) may inadvertently be traversed [Figure 2a-c]. If the contralateral system is occluded distally, then bile will fl ow through the needle tract and out through the puncture site or into the ipsilateral system [Figures 3 and 4].
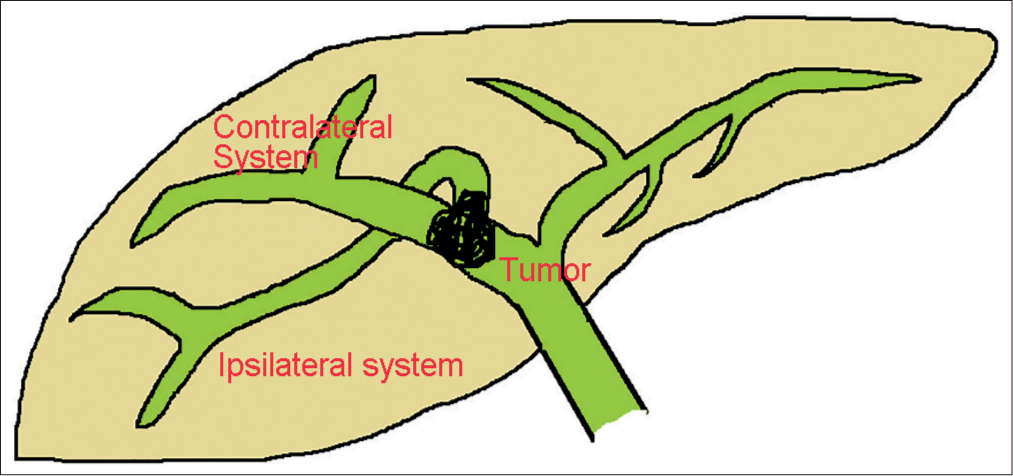
- Biliary separation by a tumor at the confl uence. The tumor has obstructed and separated two main branches of the biliary tract.

- Ipsilateral biliary decompression. (a) The needle normally enters into a dilated branch, however, sometimes the needle punctures a small branch of an adjacent obstructed biliary branch called contralateral system. (b) A hydrophilic catheter directed and passed from the stricture. (c) The stent has deployed at the stricture site.

- Stent occlusion due to thrombosis and debris. This schematic picture shows clot/debris as red materials in the stent lumen obstructing the ipsilateral system. This may occur shortly after stenting. This schematic picture also shows how bile drains from the ipsilateral system to the skin surface due to its high pressure after stent obstruction. This high pressure causes the trajectory tract to remain patent. As a result, bile leakage at the puncture site does not stop.
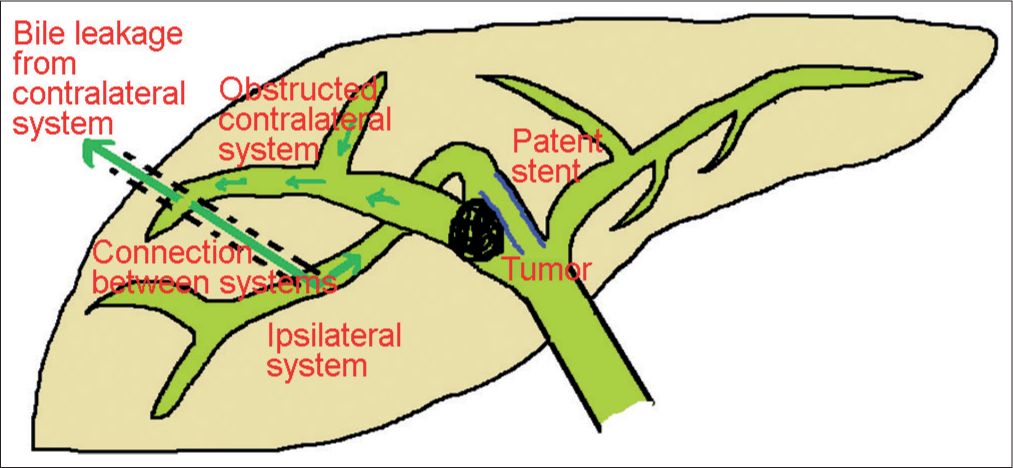
- Skin bile leak after biliary decompression. (a) Mechanism of bile leak in the absence of stent occlusion. Note that bile fl ow appears when high-pressure bile of the contralateral system fi nds its way via trajectory line to the lower pressure sites e.g. to the skin surface and ipsilateral stented biliary system (dark green arrows).
Bile leakage onto the skin can pose quite a problem for patients [Figure 5]. The caustic nature of bile results in skin irritation, and patients often have to wear a small ostomy appliance at their puncture site. Additionally, diversion of bile from the enterohepatic cycle may cause digestive problems. We reviewed 264 patients who underwent percutaneous biliary decompression between 2000 and 2013, of whom 16 patients developed bile leak at their puncture site. Here we review the causes for bile leak as well as treatment approaches.

- 68-year-old man with cholangiocarcinoma who presented with bile leaks at the puncture site. Note that the content of secretions is pure bile.
MATERIALS AND METHODS
This retrospective study reviewed 264 patients, above the age of 18, between 2000 and 2013 with non-resectable malignant tumors resulting in biliary obstruction requiring percutaneous biliary decompression. Of these patients, 16 developed percutaneous bile leak. Patients with incomplete records were excluded from the study. The Ethics Committee of the affiliated University of Medical Sciences approved this review. Informed consent was obtained from all patients prior to any procedure.
Our institutional preference is a two-stage biliary decompression. Patients are kept fasting for at least 8 h, and 1 g of intravenous ceft riaxone is administered at least 12 h before the procedure. An 18-gauge, 20-cm Chiba-type needle (Meditech Devices Ahmedabad, India) is introduced into a peripheral bile duct under ultrasound guidance. Contrast is injected through the needle under fl uoroscopy to confi rm placement in a bile duct. A 0.035″ 150-cm hydrophilic guide wire (Terumo, Tokyo, Japan) is advanced through the needle into the central bile ducts. The needle is removed, and the tract is dilated, and an 8Fr pigtail catheter (Bioteq, GmbH, Muenster, Germany) is placed.
The patients would return after 2 days for stent placement. A hydrophilic guide wire is passed through the existing catheter, which is exchanged for a 9 Fr, 11-cm dilator sheath (Telefl ex, Wayne, Pennsylvania, USA). A bare metallic stent (Endofl ex Voerde, GmbH, Muenster, Germany) is then deployed into the stricture [Figure 6]. The stricture would be dilated by an 8 × 40-mm-diameter balloon (Optimed, Ettlingen, Germany) if the stent is unable to self-expand.

- 64-year-old male patient with cholangiocarcinoma who presented with biliary obstruction. (a) Fluoroscopic cholangiogram of the liver in anteroposterior view shows the hydrophilic guide wire in the posterior branch. It has passed the stricture and its tip is seen in the duodenum. (b) Stent deployment at the obstruction site.
After stent placement, an 8 Fr pigtail catheter (internal– external) would be placed for fl ushing and also for performing the cholangiography. The patients were then observed for another 2 days to monitor bile pressure via the dilator sheath or catheter. The stent was determined to be patent if the pressure was less than 2 cm H2O after 2 days, and the dilator sheath and catheter would be removed. Procedure success was defi ned as a decrease of at least 30% in the bilirubin level within 48–72 h.
Patients who had persistent puncture site bile leakage after 24 h were considered to have a bile leak. In these patients, 350 mg/mL dilute Omnipaque (GE Healthcare AS, Oslo, Norway) was injected into the puncture tract via an 8 Fr blunted-head feeding catheter (Supa, Tehran, Iran). The stent was irrigated and ballooned if the stent appeared occluded.
For patients with patent stents, an internal–external biliary drain was placed through the stent [Figure 7a and b]. Despite adequate drainage of the ipsilateral system, these patients had severe bile leak continued from the catheter site at the skin. We concluded that there must be a connection between a blocked biliary compartment (the contralateral system) and the needle tract due to low biliary pressure measurements taken at the tip of the internal–external drain in the ipsilateral compartment.
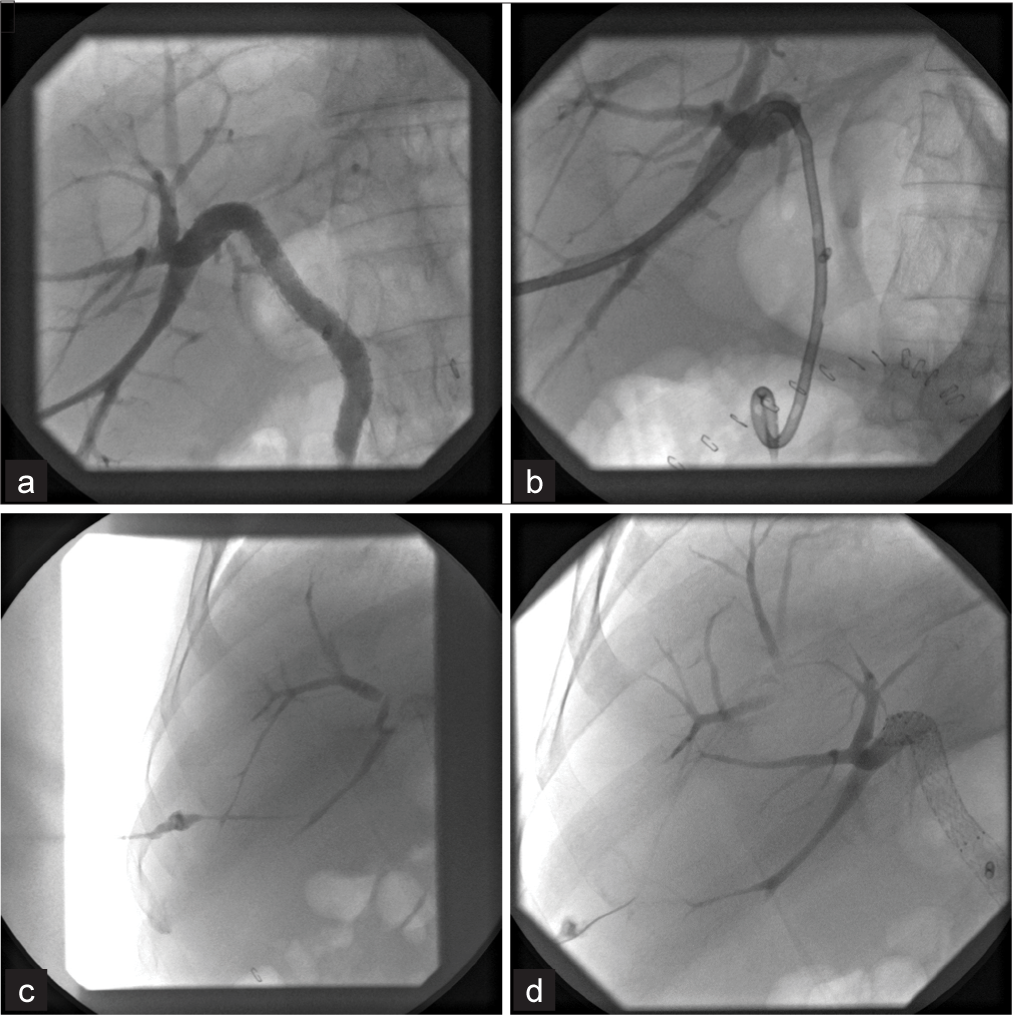
- 64-year-old male patient with cholangiocarcinoma who presented with biliary obstruction, underwent transhepatic biliary decompression and developed a severe leak at the puncture site. (a) A fluoroscopic cholangiogram in the A-P view using a catheter reveals that the stent was patent. (b) Fluoroscopy of the liver in the A-P view shows that internal-external biliary drainage was inserted to treat biliary leak, but the leak continued from the side of the catheter at the puncture site. (c) Fluoroscopic cholangiogram in the A-P view using a syringe via the orifice shows that the trajectory tract is connected to a side branch of the anterior division of right bile ducts which continues and connected to the obstructed hilum. (d) Fluoroscopy of the liver in the A-P view shows that a hydrophilic wire is entering and directing to the anterior segment branch for stenting of the hilar part. After the anterior branch decompression, bile leakage stopped in this patient.
Subsequently, the internal–external biliary drain was removed, and contrast was injected into the drain tract via a syringe [Figure 7c and d]. This demonstrated a connection between an adjacent obstructed biliary system (the contralateral system) and the catheter tract. These patients then underwent PTBD of the contralateral biliary system. Treatment success was determined by cessation of bile leak after 24 h.
RESULTS
Sixteen of 264 patients who underwent percutaneous biliary decompression developed bile leakage at the puncture site. Nine of these patients were male. The average patient age was 58. Twelve of these patients demonstrated an occluded biliary stent, and their bile leak resolved after irrigation and ballooning.
Four patients with bile leak demonstrated patent biliary stents and persistent leakage despite internal–external biliary drain placement. Cholangiograms in these patients demonstrated connections from the stented biliary system (the ipsilateral system), branches of a different occluded biliary system (the contralateral biliary tract), and the drain tract. All four patients underwent PTBD of the contralateral biliary system with subsequent resolution of their bile leak.
DISCUSSION
PTBD is a relatively common procedure for biliary obstruction. One of the complications of PTBD is bile leakage around the puncture site. Over a 13-year period, 16 patients developed bile leak at the puncture site after PTBD at our institution. Four of these patients were found to have patent stents and fistulous connections between the drained biliary system (the ipsilateral system) and a separate obstructed biliary system (the contralateral system). To the best of our knowledge, there have not been any reports regarding this mechanism for puncture site bile leak after PTBD.
We would like to refer to this mechanism of bile leak “Yo- Yo reflux” for this pattern of cholangiography. However, it should not be confused with urinary Yo-Yo reflux. The Yo-Yo reflux mechanism of bile leaks occurs when a small branch from the adjacent separated contralateral system is transgressed inadvertently during ipsilateral biliary drainage. High-pressure bile fluid from the obstructed system flows through the lower pressure ipsilateral system and through the cannulation tract and onto the skin surface [Figure 7c]. It is noteworthy that in the current study, the contralateral system was not necessarily the opposite lobe, and it is usually an adjacent branch from the same lobe separated by the tumor, i.e., a right anterior branch versus an obstructed right posterior branch.
Understanding of the mechanisms of bile leaks after biliary decompression is paramount since choosing an appropriate treatment. In the case of stent occlusion, irrigation/ ballooning easily resolves the problem. However, in the Yo-Yo mechanism, stenting of the contralateral side is the only treatment. Contralateral stenting decompression should be performed through the fistula and via that small branch of contralateral system punctured unintentionally as an access site [Figure 7d].
One of the advantages of our two-stage biliary decompression is that a fistulous tract is created within a few days by the pigtail catheter. This acts as an access route for diagnostic and therapeutic procedures. The fistula eventually closes when adequate biliary drainage is established and is not considered a cause of bile leak. An additional benefit of the temporary fistula tract is that it prevents overflowing bile from entering the peritoneum as it acts as a low-resistance pathway for overflowing bile. Because of these reasons, we strongly recommend two-stage biliary decompression.
CONCLUSION
Patients with non-resectable malignant biliary obstruction often need biliary decompression. Decompression of the biliary system preserves liver function, prevents cholangitis, improves survival, and improves quality of life. After excluding traumatic leak and other non-bilious leaks, there are two mechanisms of bile leak at the puncture site: stent occlusion and Yo-Yo reflux. If an injection of contrast by a catheter inside the skin fistula did not show the cause of the biliary leak, the injection should be performed into the orifice of the fistula by a syringe to reveal Yo-Yo reflux. Differentiation of causes is crucial as treatments are different.
Acknowledgment
We thank our patients for their cooperation and also our colleagues for their assistance.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Criteria of unresectability and the decision-making process. HPB. 2008;10(2):122-5.
- [CrossRef] [PubMed] [Google Scholar]
- Current status of percutaneous transhepatic biliary drainage in palliation of malignant obstructive jaundice: A review. Indian J Palliat Care. 2016;22(4):378.
- [CrossRef] [PubMed] [Google Scholar]
- Cholangiocarcinoma: Current knowledge and new developments. Gut Liver. 2017;11(1):13.
- [CrossRef] [PubMed] [Google Scholar]






