Translate this page into:
Geniculate artery embolization for the treatment of refractory hemarthrosis following meniscal repair

*Corresponding author: Monika Neale, Kansas City University, Joplin, Missouri, United States. mneale@kansascity.edu
-
Received: ,
Accepted: ,
How to cite this article: Neale M, Grzybowski RF, Rea W, Greiner B. Geniculate artery embolization for the treatment of refractory hemarthrosis following meniscal repair. Am J Interv Radiol 2022;6:9.
Abstract
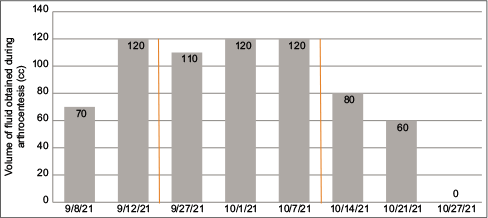
The present case report describes a unique example of recurrent hemarthrosis and associated arthralgia in a 41-year-old male after laparoscopic left medial meniscus repair, which failed to resolve with conservative treatment and surgical revision. Due to the worsening symptomatology as evidenced by increasing volume of aspirated blood during serial arthrocenteses and gradually decreasing range of motion of the joint despite surgical revision, geniculate artery embolization (GAE) was recommended. GAE is not routinely utilized to treat postoperative complications following meniscus repair; however, in the present case, utilizing selective angiographic embolization of the geniculate arteries led to successful treatment of recurrent spontaneous hemarthrosis and associated arthralgia. At this point, the patient has been symptom free for nine months. Relevant patient history, along with progress monitoring data from follow-up visits, demonstrates that spontaneous hemarthrosis and associated arthralgia following laparoscopic medial meniscus repair may be successfully treated with GAE. This is a noteworthy finding which underlines the importance of investigating alternative therapies in treatment refractory cases. However, a thorough evaluation of the appropriateness of this intervention is of paramount importance and its potential benefits need to be determined on a case-by-case basis.
Keywords
Arthralgia
Geniculate artery embolization
Medial meniscus repair
Treatment refractory recurrent hemarthrosis
INTRODUCTION
An increasing number of publications in minimally invasive vascular procedures discuss the utility of geniculate artery embolization (GAE) to resolve recurrent hemarthrosis following total knee arthoplasty (TKA), and the number of publications about the utility of GAE for pain management in osteoarthritis is on the rise as well (Bagla et al., 2020). However, little evidence is available regarding the effectiveness of GAE in the management of post-surgical complications following laparoscopic meniscus repair. This may be attributable to the fact that recurrent hemarthrosis following medial meniscus repair is a relatively uncommon postoperative complication. While arthroscopic meniscal debridement and repair are two of the most commonly performed surgical procedures in the United States, their associated complication rate is reported to be approximately 1%.[1] Clinical outcomes following meniscus repair quantified by healing rates and post-operative complications were found to be favorable regardless of suturing technique used, as reported by a meta-analysis of six studies.[2]
CASE REPORT
A 41-year-old male patient underwent an uneventful medial meniscus repair of the left knee in September 2021 following a traumatic knee injury in July of the same year. Following meniscal repair, his pain and mobility did not improve with the combination of rest, anti-inflammatory medication, over-the-counter oral analgesics, and physical therapy, which ultimately prompted surgical repair. The patient’s medical history was non-contributory. His surgical history was significant for numerous athletic injuries and surgical repairs involving the lower back, bilateral shoulders, and right elbow. Five days after the meniscal repair procedure, the patient presented with severe left knee pain and swelling secondary to hemarthrosis for the 1st time without any identifiable precipitating factor. His symptoms were treated with arthrocentesis and 70 cc of bloody fluid was aspirated.
The patient then returned several days later with recurrence of symptoms, describing his pain as “excruciating” despite post-operative pain management with prescription opioids. Repeat arthrocentesis was performed, yielding 120 ml of bloody aspirate. Aspirate cultures showed no evidence of septic arthritis. Serum hematologic and biochemical analyses were within normal limits and coagulation studies did not reveal coagulopathies. Consequently, the decision was made to perform an arthroscopic synovectomy combined with arterial cauterization. Two additional arthrocenteses were performed: One at the time of the revision surgery and a subsequent procedure 4-day post-operative, each yielding between 110 and 120 cc of bloody aspirate [Table 1]. Despite the revision surgery, the patient continued to experience recurrent hemarthrosis with associated severe arthralgia, as well as limited mobility of the knee. He was then referred to interventional radiology for an arteriogram of the left lower extremity with GAE.
 |
Before performing the arteriogram, 100 cc of bloody fluid was aspirated from the patient’s left knee. Then, using real-time ultrasound guidance, antegrade access into the left common femoral artery was obtained. The remainder of the examination was performed using fluoroscopic guidance.
A similar procedure was described by various authors, including Bagla et al.[3,4] for recurrent hemarthrosis following TKA and Sajan et al. for pain management in osteoarthritis.[5]
A 5 French Kumpe catheter (Cook Medical, Bloomington, IN) and 0.035 inch advantage Glidewire (Terumo, Somerset, NJ) were used to selectively catheterize the distal left superficial femoral artery and an angiogram centered over the knee to evaluate the left superficial femoral, popliteal, tibial, and geniculate arteries. A proximal trifurcation of arteries was observed from this injection. Using the 5 French Kumpe catheter as a coaxial guide catheter, a 2.8 French Progreat microcatheter and 0.018 microwire (both Terumo, Somerset, NJ) were then used to selectively catheterize the left superior medial genicular artery and a superior medial genicular artery angiogram was performed. A marked contrast “blush” was noted [Figure 1a] corresponding to synovial hyperemia. Embolization of the superior medial genicular artery was then performed using 100–300 μm Embosphere microspheres (Merit Medical, South Jordan, Utah) with the endpoint being sluggish flow within the artery as demonstrated on a follow-up selective medial genicular artery angiogram [Figure 1b].
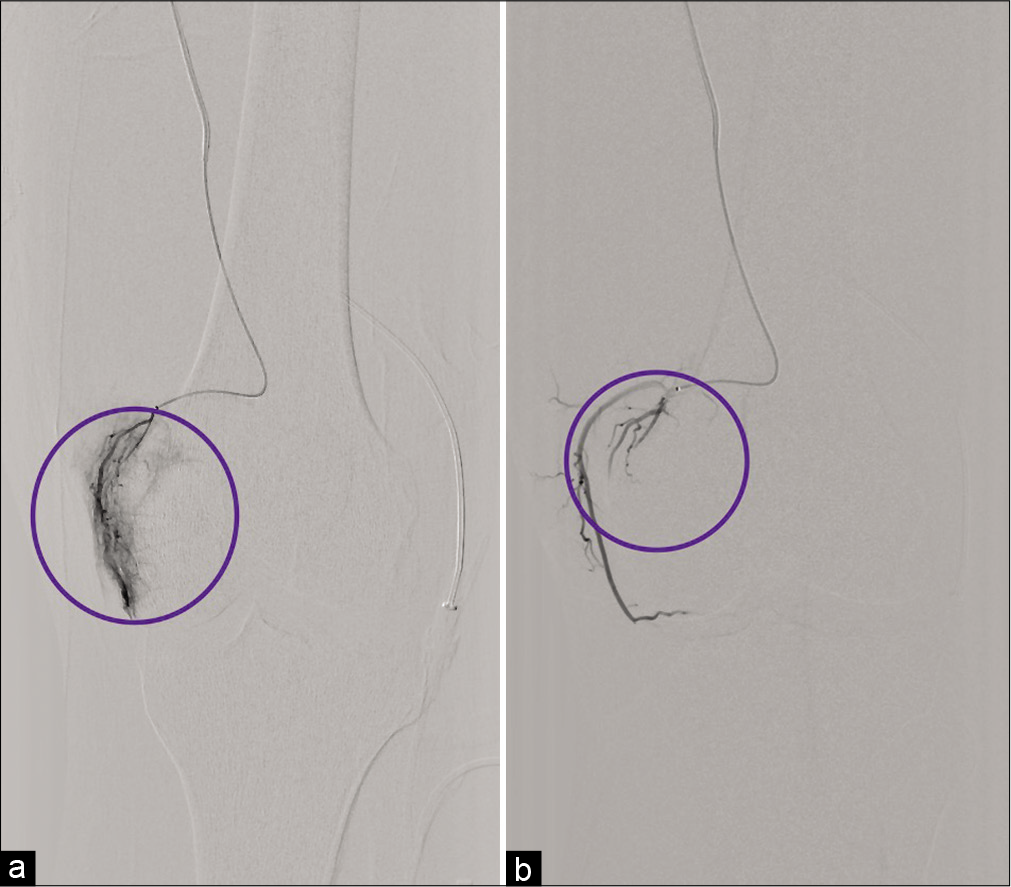
- (a) 41-year-old male with a recent history of medial meniscal repair of the left knee presented with recurrent spontaneous hemarthroses that failed to resolve with conservative management and surgical revision. Digital Subtraction Angiograph (DSA) of the left superior medial geniculate artery before embolization. The circled area demonstrates significant vascularization (blush) of the medial geniculate artery. (b) Patient is the same 41-year-old male with recurrent spontaneous hemarthrosis following meniscal repair undergoing GAE. Post-embolization DSA of the left superior medical geniculate artery. Selective angiography of the left superior medial geniculate artery depicts devascularization highlighted by the circle.
Selective catheterization, angiogram, and embolization of the lateral superior geniculate artery were performed in a similar fashion [Figure 2a and b].

- (a) 41-year-old male with a recent history of medial meniscal repair of the left knee presented with recurrent spontaneous hemarthroses that failed to resolve with conservative management and surgical revision. Digital Subtraction Angiograph (DSA) selectively targeting the left superior lateral geniculate artery before embolization. Hypervascularization is indicated by the blue arrow. (b) Post-embolization DSA of the left superior lateral geniculate artery in the same 41-year-old male patient demonstrates a notable reduction in hyperemia indicated by the blue arrow.
Selective catheterization of the inferior lateral geniculate artery with the Progreat microcatheter (Terumo, Somerset, NJ) and 0.014 Fathom microwire (Boston Scientific, Marlborough, MA) was then performed followed by an inferior lateral genicular artery angiogram. A marked contrast “blush” was noted corresponding to synovial hyperemia. Embolization of the inferior lateral genicular artery was then performed with the endpoint being sluggish flow within the artery and this was demonstrated on a follow-up selective inferior lateral genicular artery angiogram. The medial inferior geniculate artery was not embolized.
On completion of the embolization, all catheters were removed. A total of 7.5 ml of Embosphere microspheres (Merit Medical, South Jordan, Utah) were used. An Angio-Seal device (Terumo, Somerset, NJ) was deployed for successful closure of the left common femoral arteriotomy. Following conclusion of the arteriogram and embolization, additional 15–20 cc of bloody fluid was aspirated from the left knee. The resolution of the hyperemia is demonstrated by the pre- and post-procedure Digital Subtraction Angiographs, as shown in [Figure 3a and b].

- (a) 41-year-old male with a recent history of medial meniscal repair of the left knee, who developed persistent swelling, arthralgia, and limited range of motion following meniscal repair. He presented with recurrent spontaneous hemarthroses that failed to resolve with conservative management and surgical revision. Diffuse synovial hyperemia was identified through Digital Subtraction Angiograph (DSA). Hypervascularization of the left medial and lateral superior geniculate arteries is highlighted in blue and pink circles, respectively. Hypervascularization of the left inferior lateral geniculate artery is marked by the yellow circle. (b) A post-embolization DSA image from the same 41-year-old male patient demonstrates diminished contrast blush in the areas of the left medial superior geniculate artery (blue circle), lateral superior geniculate artery (pink circle), and lateral inferior geniculate artery (yellow circle). The left medial inferior geniculate artery was not accessed.
The patient tolerated the procedure well, with no immediate major post-procedural complication. He, however, experienced minor discomfort associated with mild bruising and transient cutaneous erythema at the puncture site, which was managed conservatively. There were no new skin changes noted at the embolization sites. He was discharged home after two hours of observation. He was then evaluated multiple times over the following six weeks with no complications reported. At the one-week and two-week follow-ups, additional arthrocenteses were performed, yielding 80 cc and 60 cc of blood, respectively [Table 1]. Ultrasound imaging no longer demonstrated fluid collection at the three-week follow-up. At that time, the patient reported marked improvement in arthralgia and knee mobility. Physical examination showed a lack of effusion recurrence at three weeks and six weeks following GAE, although full range of motion was not achieved at the 6-week mark.
DISCUSSION
In the occurrence of recurrent hemarthrosis, the clinical course and outcome of recurrent hemarthrosis following meniscus repair are expected to be similar to that of TKA.[6] When recurrent hemarthrosis is a post-operative complication and is not attributable to an identifiable vascular injury or coagulopathy, as in this patient’s case, the majority of cases respond well to traditionally employed conservative management techniques.[7] Conservative treatment options for spontaneous recurrent hemarthrosis include arthrocentesis[7] and rest combined with icing, compression, and elevation[8] which typically results in symptom resolution in over 80% of cases. However, this patient did not respond favorably to conservative management. Consequently, based on the similar course and outcome[6] between recurrent hemarthrosis following TKA and recurrent hemarthrosis following meniscal repair, as well as the effectiveness of GAE in the treatment of recurrent hemarthrosis after TKA, GAE was a reasonable treatment choice for this patient.
CONCLUSION
Based on progress monitoring data on arthrocentesis volumes and subjective reports of pain, the present case report suggests that refractory spontaneous hemarthrosis and associated arthralgia following laparoscopic medial meniscus repair may be successfully treated with GAE. Therefore, we can conclude from this case report that GAE can effectively mitigate hemarthrosis not only associated with TKA but also hemarthrosis following meniscus repair and synovectomy in the native knee. Based on the outcomes of this case, it can be further hypothesized that GAE may be a viable treatment option for recurrent spontaneous hemarthrosis following other surgical procedures in the native knee as well.
AUTHORS CONTRIBUTIONS
All authors have read and approved the final manuscript.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
No funding was received to assist with the preparation of this manuscript.
Conflicts of interest
The authors have no financial or proprietary interest in any materials discussed.
References
- Geniculate artery embolization in the management of spontaneous recurrent hemarthrosis of the knee: Case series. J Vasc Interv Radiol. 2013;24:439-42.
- [CrossRef] [PubMed] [Google Scholar]
- Complications after arthroscopic knee surgery. Am J Sports Med. 2014;42:292-6.
- [CrossRef] [PubMed] [Google Scholar]
- Traditional investigation and management for recurrent hemarthrosis after total knee arthroplasty: A case report. World J Clin Cases. 2020;8:1966-72.
- [CrossRef] [PubMed] [Google Scholar]
- A systematic review and meta-analysis of arthroscopic meniscus repair in young patients: Comparison of all-inside and inside-out suture techniques. Knee Surg Relat Res. 2019;31:1-11.
- [CrossRef] [PubMed] [Google Scholar]
- Genicular artery embolization for the treatment of knee pain secondary to osteoarthritis. J Vasc Interv Radiol. 2020;31:1096-102.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of recurrent hemarthrosis after total knee arthroplasty. Knee Surg Relat Res. 2018;30:147-52.
- [CrossRef] [PubMed] [Google Scholar]
- Musculoskeletal interventions: A review on genicular artery embolization. Semin Intervent Radiol. 2021;38:511-4.
- [CrossRef] [PubMed] [Google Scholar]
- Update on the risks of complications after knee arthroscopy. BMC Musculoskelet Disord. 2018;19:179.
- [CrossRef] [PubMed] [Google Scholar]







