Translate this page into:
Transient Aortoiliac Narrowing during Voluntary Valsalva Maneuver

*Corresponding Author: Pushpender Gupta, Departments of, Radiology, Kadlec Regional Medical Center, 888 Swift Blvd, Richland, 99352 United States. E-mail: drpushpender@gmail.com
-
Received: ,
Accepted: ,
How to cite this article:Habbu A, Bawa P, Hatti K, Gupta P. Transient Aortoiliac Narrowing during Voluntary Valsalva Maneuver. Am J Interv Radiol 2019; 3(7) 1-3.
Abstract
A 54-year-old male presented to the outpatient surgery clinic with chronic intermittent right inguinal pain. An unenhanced computed tomography (CT) scan during Valsalve maneuver was performed, which demonstrated aortoiliac narrowing. Kinking of the duodenum and renal vasculature, and flattening of the inferior vena cava and iliac vasculature were also noted. A CT angiogram was subsequently performed without Valsalva maneuver which demonstrated complete resolution of the vascular and enteric findings. The case demonstrates that transient aortoiliac narrowing can also occur during voluntary Valsalva maneuver. Awareness of this entity is important so that patients can be reassured about the transient physiologic nature of these findings.
Keywords
Valsalva maneuver
Aortoiliac narrowing
Computed tomography
Transient
INTRODUCTION
Aortoiliac occlusive disease is most commonly seen in atherosclerosis. Inflammatory disorders resulting in aortitis may also result in severe aortic disease. Voluntary Valsalva maneuver utilized during computed tomography (CT) scan has not been previously reported to cause such critical aortic narrowing. We present a case of transient severe long segment narrowing of the abdominal aorta and iliac arteries secondary to Valsalva maneuver. Awareness of this entity is important so that patients can be reassured about the physiologic nature of these findings.
CASE REPORT
A 54-year-old male presented to the outpatient surgery clinic with chronic intermittent right inguinal pain for 3 years. The pain was 9/10 in maximum severity, sharp in nature, and radiated to the right lower quadrant. The pain increased with exercise and decreased with rest. The patient reported no history of extremity claudication. The medical history was significant for thyroid disease. The surgical history was significant for appendectomy and right inguinal hernia repair. Significant medication use included levothyroxine for the thyroid disease. The vital signs included blood pressure of 128/76 mmHg, pulse rate of 63 beats per minute, and SpO2 of 98%. The physical examination demonstrated no evidence of recurrent right inguinal hernia. No mass or bulging noted in the area of concern. The rest of the physical examination was within normal limits. Due to clinical suspicion of occult recurrent right inguinal hernia, an unenhanced abdominal CT during Valsalva maneuver was performed [Figure 1].
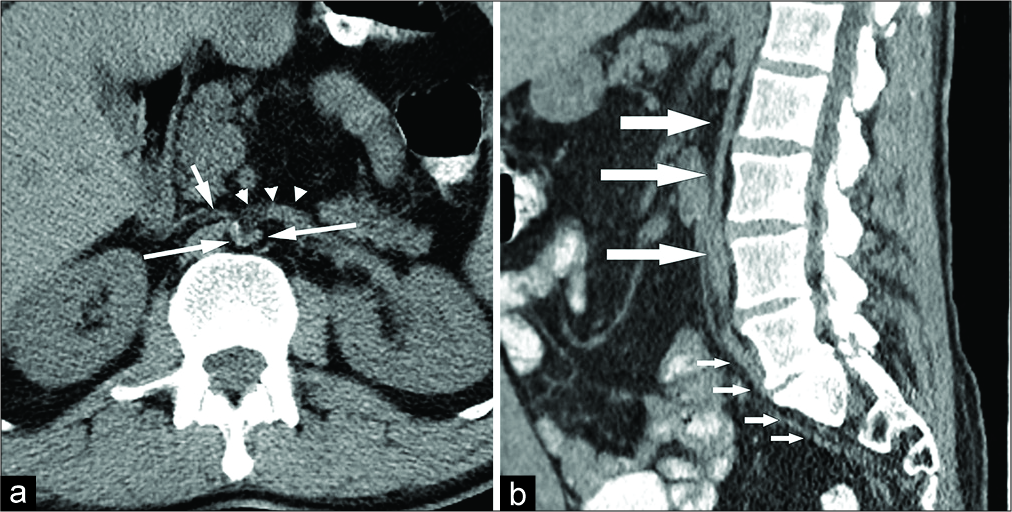
- A 54-year-old male who presented with chronic intermittent right inguinal pain. (a) Unenhanced axial computed tomography (CT) image of the abdomen during Valsalva maneuver at the level of the third portion of the duodenum shows V-shaped configuration of the abdominal aorta (long arrow) and flattening of the inferior vena cava (short arrow). The duodenum (arrowhead) is kinked. (b) Unenhanced sagittal reformatted CT image of the abdomen and pelvis shows severe long segment narrowing of the abdominal aorta (long arrows) and the iliac arteries (short arrows).
The unenhanced abdominal CT during Valsalva maneuver shows severe long segment narrowing of the abdominal aorta with V-shaped appearance on the axial images [Figure 1a]. Severe narrowing of the aorta and iliac arteries is noted on the sagittal reformats [Figure 1b]. The third portion of the duodenum is kinked, projecting between two limbs of the V-shaped abdominal aorta [Figure 1a]. Flattening of the inferior vena cava is also seen [Figure 1a]. However, no arterial collaterals were visualized. Minimal atherosclerosis is seen. There is no intra-abdominal soft tissue edema, hemorrhage, ascites, or mass causing vascular compression. There is no aortic wall thickening or para-aortic inflammation.
In view of the complaints of severe right inguinal pain, critical aortic narrowing, and additional vascular and mesenteric findings mentioned above, a CT angiogram (CTA) of the abdomen and pelvis with bilateral lower extremity runoffs was performed without Valsalva maneuver. The CTA demonstrates complete resolution of aortic narrowing and other vascular and enteric findings. The aorta is widely patent [Figure 2]. The inferior vena cava (IVC) is normal in caliber [Figure 2a]. There is no kinking of the duodenum [Figure 2a]. The iliac arteries appear widely patent [Figure 2b]. The findings were thus found to be transient and hence physiologic in nature. The patient was reassured accordingly.

- A 54-year-old male who presented with chronic intermittent right inguinal pain. (a) Contrast-enhanced axial computed tomography (CT) angiography image of the abdomen at the level of the third portion of the duodenum shows resolution of the aortic narrowing. The aorta appears widely patent (long arrows). The duodenum is normal in appearance without kinking (short arrows). (b) Contrast- enhanced sagittal reformatted CT angiography image of the abdomen and pelvis shows widely patent abdominal aorta (long arrows) and iliac arteries (short arrows).
DISCUSSION
CT imaging to evaluate for an abdominal wall hernia is commonly performed as a single-phase acquisition utilizing Valsalva maneuver. In 2005, Jaffe et al. studied 100 patients who underwent CT studies with and without Valsalva maneuver. The authors concluded that a single-phase CT scan performed during Valsalva maneuver is sufficient to detect 100% abdominal wall hernias.[1]
Kawabata et al. measured the increase in intra-abdominal pressure during voluntary Valsalva in 10 highly trained male judo athletes and 11 healthy men, who performed standardized isometric lifting efforts.[2] The study showed that there was an increase in the maximal intra-abdominal pressure during Valsalva up to a mean of 204 ± 50 mmHg in trained male athletes and 140 ± 37 mmHg in healthy men, measured in standing position using intrarectal transducer.[3] Cobb et al. measured maximum intra-abdominal pressure at 64 mmHg (mean – 39.7 mmHg, minimum – 20 mmHg, and SD – 11 mmHg) in healthy volunteers during Valsalva maneuver at rest, in supine position. The increase in intra-abdominal pressure was highest during jumping and coughing.[3]
In a normal healthy adult, the mean systolic blood pressure within the aorta measured using aortic pressure sensor in proximal ascending aorta (at rest, in supine position) has been demonstrated to be 117 ± 3 mmHg during systole, 77 ± 2 during diastole, and 96 ± 2 as mean pressure.[4] Valsalva maneuver is associated with significant hemodynamic changes including hypotension in Phase II due to decreased cardiac venous return and decreased cardiac output resulting from increased intrathoracic pressure.[5]
Thus, Valsalva maneuver has a potential to increase intra- abdominal pressure above the aortic diastolic pressure, occasionally causing aortic compression, although the imaging literature documenting this is scarce. Krol and Hallett reported CT findings of flattening of abdominal aorta, IVC, and iliac vessels in a patient due to involuntary Valsalva maneuver.[6] The patient had an episode of vomiting during CT image acquisition resulting in findings similar to the present case.
Aortoiliac occlusive disease can result either from an intrinsic aortic pathology such as atherosclerosis or large vessel vasculitis (e.g., Takayasu arteritis) or an extrinsic pathology resulting in aortic compression/encasement. The extrinsic causes typically can include retroperitoneal mass, retroperitoneal fibrosis/aortitis, or, as in our case, elevation of the intra-abdominal pressure.[7-9]
Takayasu arteritis is a necrotizing granulomatous large vessel panarteritis, which primarily involves the aorta and major aortic branches. Abdominal aorta is the most common segment of the aorta involved. Takayasu arteritis most commonly occurs in young women (the second and third decade). Typical CTA findings include concentric thickening of the wall of the aorta, which may show double ring enhancement pattern due to thickened poorly enhancing intima and outer thickened enhancing media and adventitia. Additional CTA findings include long segment concentric tapered luminal narrowing (“rat tail” appearance), occlusion, branch vessel (renal, carotid, and subclavian arteries) involvement, wall calcification, ectasia, and aneurysm.[7,8] In our case, there was minimal atherosclerosis, but no evidence of abnormal aortic wall thickening or enhancement.
Retroperitoneal fibrosis or chronic periaortitis is characterized by mass-like retroperitoneal periaortic fibrosis, which can cause aortic stenosis. The fibrosis is usually anterior and lateral to aorta. The posterior aspect of aorta is usually spared. There is often encasement of IVC and both ureters.[9] No retroperitoneal fibrosis or mass was visualized in our case.
CONCLUSION
Increased intra-abdominal pressure during voluntary Valsalva maneuver can rarely result in aortoiliac narrowing. Diagnostic clues to this entity include history of Valsalva maneuver during CT image acquisition, diffuse arterial and venous narrowing, absence of secondary findings of bowel ischemia, absence of aortic wall thickening or para-aortic inflammation, absence of intra-abdominal hemorrhage, ascites, inflammation, or mass should help in differentiation of physiological narrowing from pathological aortic occlusion. In our opinion, when physiologic narrowing is suspected, repeat limited CT images of the abdomen without Valsalva maneuver (if the patient is still on scanner) may be considered to confirm physiological nature of the findings. Alternatively, Doppler ultrasound evaluation of the aorta may be considered, thus avoiding radiation and contrast exposure from CTA.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- MDCT of abdominal wall hernias: Is there a role for valsalva's maneuver? AJR Am J Roentgenol. 2005;184:847-51.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in intra-abdominal pressure and spontaneous breath volume by magnitude of lifting effort: Highly trained athletes versus healthy men. Eur J Appl Physiol. 2010;109:279-86.
- [CrossRef] [PubMed] [Google Scholar]
- Normal intraabdominal pressure in healthy adults. J Surg Res. 2005;129:231-5.
- [CrossRef] [PubMed] [Google Scholar]
- Aortic input impedance in normal man: Relationship to pressure wave forms. Circulation. 1980;62:105-16.
- [CrossRef] [PubMed] [Google Scholar]
- The valsalva manoeuvre cardiovascular effects and performance technique: A critical review. Respir Physiol Neurobiol. 2005;147:39-49.
- [CrossRef] [PubMed] [Google Scholar]
- Transient, marked flattening of the abdominal aorta, iliac arteries, and venous structures during active vomiting: Report of a case demonstrated by MDCT. Abdom Imaging. 2011;36:582-5.
- [CrossRef] [PubMed] [Google Scholar]
- Aortic stenosis: Spectrum of diseases depicted at multisection CT. Radiographics. 2003;23:S79-91.
- [CrossRef] [PubMed] [Google Scholar]
- Aortitis: Imaging spectrum of the infectious and inflammatory conditions of the aorta. Radiographics. 2011;31:435-51.
- [CrossRef] [PubMed] [Google Scholar]
- Takayasu arteritis: Imaging spectrum at multidetector CT angiography. Br J Radiol. 2012;85:e1282-92.
- [CrossRef] [PubMed] [Google Scholar]






