Translate this page into:
Successful treatment with flow diverter for small carotid cavernous aneurysm with oculomotor palsy: A case re port

*Corresponding author: Takahiro Yokoyama, Department of Neurosurgery, Itabashi Chuo Medical Center, Itabashi, Japan. y.takahiro.0730@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Yokoyama T, Hoshino T, Nakamura S, Kawamata T. Successful treatment with flow diverter for small carotid cavernous aneurysm with oculomotor palsy: A case report. Am J Interv Radiol. 2024;8:10. doi: 10.25259/AJIR_19_2024
Abstract
The effectiveness of flow diverters (FDs) in treating small aneurysms that cause neurological symptoms remains unclear. We present a case of a small carotid cavernous aneurysm (CCA) with oculomotor palsy treated early with an FD, resulting in favorable outcomes. A 74-year-old woman presented with a rapidly progressing left pupil-sparing oculomotor palsy. Magnetic resonance imaging and computed tomography angiography demonstrated a 4-mm CCA arising from the lateral wall of the left internal carotid artery (ICA). Further, investigation suggested that the oculomotor palsy could be caused by the small CCA or benign Tolosa–Hunt syndrome. On the 4th day of admission, we initiated steroid therapy simultaneously with antiplatelet therapy for diagnosis and treatment; however, the symptoms did not improve. Consequently, on the 12th day of admission, we performed an endovascular procedure for the small CCA using an FD, expecting decreased aneurysm’s pulsation and mass effect on the oculomotor nerve. Dual antiplatelet therapy and steroid therapy were initiated simultaneously 7 days before endovascular treatment. A pipeline embolization device was deployed between the left C7 segment of the ICA, just proximal to the left anterior choroidal artery, and the C3 segment. Post-procedure digital subtraction angiography (DSA) revealed no changes in aneurysm findings. Oculomotor palsy substantially improved immediately after the procedure. The patient had an uneventful course after the procedure, and follow-up DSA after 6 months revealed complete obliteration of the aneurysm. We successfully treated a case of small CCA with oculomotor palsy using early intervention with an FD, suggesting the effectiveness of this approach in addressing small CCAs causing neurological symptoms. However, further studies are required to confirm the optimal nature of FDs.
Keywords
Carotid cavernous aneurysm
Flow diverter
Oculomotor palsy
Subarachnoid hemorrhage
INTRODUCTION
The application of a flow diverter (FD), initially adapted as a device for treating large and giant wide-necked aneurysms, has expanded to treating smaller aneurysms due to its safety and effectiveness. However, its efficacy in treating extracranial aneurysms causing neurological symptoms remains unclear. Herein, we present a case of a small carotid cavernous aneurysm (CCA) with oculomotor palsy that was treated early with flow diversion, resulting in favorable outcomes.
CASE REPORT
A 74-year-old woman, without a family history of cerebral aneurysms or subarachnoid hemorrhage, presented with dull pain behind both eyes and binocular diplopia. Despite exhibiting no visible abnormalities on physical examination, the diplopia gradually deteriorated over 5 days, while the pain improved. Left oculomotor palsy was noted, and the patient was referred to our hospital where left pupil-sparing oculomotor palsy was observed [Figure 1]. The binocular diplopia impeded the patient’s walking ability. Comorbidities included hypertension and dyslipidemia, but not diabetes. A blood test revealed a hemoglobin HbA1c level of 6.0% without signs of inflammatory response.

- A 74-year-old woman with binocular diplopia. Preprocedural physical findings indicating left oculomotor palsy. A left ptosis and left eye abduction in the primary position are visible. The left eye’s adduction, elevation, and depression are limited. The pupils are equal and round with normal pupillary reflexes. These findings indicate left pupil-sparing oculomotor palsy.
Magnetic resonance imaging (MRI) and computed tomography angiography demonstrated a CCA (diameter <4 mm) arising from the lateral wall of the left internal carotid artery (ICA). However, no ischemia, mass lesions, dural arteriovenous fistula, or carotid cavernous fistulas were observed [Figure 2]. Although this small CCA may have caused oculomotor palsy, we considered alternative causes as the size of the aneurysm appeared extremely small to cause oculomotor palsy and pupil-sparing oculomotor palsy through aneurysm compression alone is atypical. Hospitalization was recommended for further investigation and treatment.
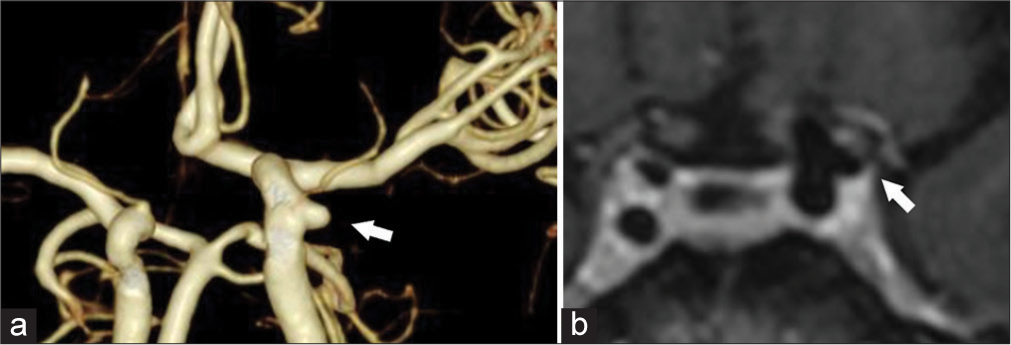
- A 74-year-old woman with a left pupil-sparing oculomotor palsy. (a) Computed tomography angiography demonstrating a small carotid cavernous aneurysm (CCA) from the lateral wall of the internal cerebral artery (width, 3.3 × 4.0 mm; height, 3.0 mm without bleb) (white arrows). (b) Contrast-enhanced magnetic resonance imaging in the axial view revealing the left CCA attached to the lateral wall of the cavernous sinus (white arrows). No surrounding inflammation or findings of enhanced lesions infiltrating the cavernous sinus, indicating Tolosa–Hunt syndrome, were observed.
Potential causes of oculomotor palsy, such as diabetes, inflammatory diseases, infectious diseases, and tumors, were explored. Blood tests for angiotensin-converting enzyme, soluble interleukin-2 receptor, antineutrophil cytoplasmic antibody, antinuclear antibody, β-D-glucan, thyroid-stimulating hormone, and thyroid hormone yielded normal results. Contrast-enhanced MRI and cisternography revealed the left CCA to be attached to the lateral wall of the cavernous sinus, without surrounding inflammation [Figure 2]. This suggested an anatomical association with the CCA attached to the left oculomotor nerve. The findings suggested that the pupil-sparing oculomotor palsy in this case could be attributed to the small CCA, or benign Tolosa– Hunt syndrome.[1]
On the 4th day of admission, steroid therapy was initiated as part of the diagnostic and treatment approach for benign Tolosa–Hunt syndrome, starting with 30 mg prednisolone on day 1 and then tapered every 2 days (20 mg/day, 10 mg/day, and 4 mg/day). Despite 7 days of therapy, the symptoms did not improve. Consequently, on day 12 of admission, we performed the endovascular procedure for the small CCA. We opted for flow diversion, considering that an FD would be more effective than stent-assisted coiling (SAC) in decreasing the aneurysm’s pulsation and mass effect on the oculomotor nerves.
Dual antiplatelet therapy (aspirin [100 mg/day] and prasugrel hydrochloride [3.75 mg/day] was initiated simultaneously with steroid therapy 7 days before endovascular treatment. A guiding catheter (ASAHI FUBUKI 8Fr 100 cm; ASAHI INTECC, Tokyo, Japan) was guided to the left cervical ICA, and a distal access catheter (Navien 5Fr 115 cm; Medtronic, Dublin, Ireland) was guided to the C3 segment of the ICA. A microcatheter (Phenom 27 160 cm; Medtronic) was then guided from the C3 segment to the M1 segment of the left middle cerebral artery using a micro-guidewire (ASAHI CHIKAI black 14 soft tip; ASAHI INTECC). A pipeline embolization device (PED; Covidien, Irvine, CA, USA) was deployed between the left C7 segment of the ICA, just proximal to the left anterior choroidal artery, and the C3 segment [Figure 3]. We ingeniously deployed the PED to increase the metal density around the aneurysm. The post-dilation after stenting was conducted using a balloon catheter (Septer C 4 × 10 mm; Terumo Corporation, Tokyo, Japan). PED apposition was assessed using cone-beam computed tomography. Postoperative digital subtraction angiography (DSA) revealed no changes in aneurysm findings.

- A 74-year-old woman with a 4-mm carotid cavernous aneurysm (CCA). (a) Immediate preprocedural digital subtraction angiography (DSA) revealing a small CCA generated from the lateral wall of the internal cerebral artery (ICA) without the association of the left ophthalmic artery. (b) A pipeline embolization device (PED; Covidien, Irvine, CA, USA) was deployed between the left C7 segment of the ICA, just proximal to the left anterior choroidal artery, and the C3 segment. We ingeniously deployed the PED to increase the metal density around the aneurysm. The post dilation after stenting was conducted using a balloon catheter (Septer C 4 × 10 mm; Terumo Corporation, Tokyo, Japan). PED apposition was assessed using cone-beam computed tomography.
Oculomotor palsy substantially improved immediately after the procedure [Figure 4], enabling the patient to walk steadily by post-operative day 1, and the diplopia disappeared. However, postoperative MRI revealed no changes in aneurysm findings. The patient experienced no complications and was discharged on the 19th day of admission. Follow-up DSA after 6 months revealed complete obliteration (CO) of the aneurysm [Figure 5].

- A 74-year-old woman with a 4-mm carotid cavernous aneurysm. The neurological findings of the left ptosis and eye movement disorder dramatically improved immediately after the procedure. Therefore, the diplopia disappeared.

- A 74-year-old woman with a 4-mm carotid cavernous aneurysm. Digital subtraction angiography revealing complete aneurysm obliteration 6 months after stenting.
DISCUSSION
We present a successful case of flow diversion for a small CCA with oculomotor palsy, an application that is not well-established yet. The safety of FDs for small aneurysms is reportedly comparable to that of SAC.[2,3] Notably, FDs in the cavernous segment of the ICA may be safer than SAC due to fewer bifurcations and perforators, simplifying the technique.[4] As FDs are relatively new devices, future research will establish its effectiveness in treating smaller aneurysms.
The effectiveness of FDs in treating small aneurysms causing neurological symptoms, including oculomotor palsy, remains undetermined. As most research focuses on the preventive effect of rupture as the primary outcome, the suitability of FDs for aneurysms measuring <4 mm in diameter is limited due to their low rupture risk. Moreover, such aneurysms rarely cause neurological symptoms. Therefore, the effectiveness of FDs for small aneurysms with neurological symptoms is difficult to establish. However, the hemodynamic changes induced by FDs in small aneurysms may contribute to the improvement of neurological symptoms.
Zanaty et al. analyzed 167 CCAs treated with FDs or other methods, revealing that FDs resulted in a higher improvement in neurological symptoms than the other models, and a favorable occlusive rate outcome.[5] Their multivariate analysis identified predictors of no improvement, including treatments other than FDs and aneurysms >15 mm in diameter.[5] Miyachi et al. reported the benefits of FDs for symptomatic large CCAs compared with those of SAC and carotid vessel destruction.[6] FDs are considered beneficial for symptomatic large CCAs, potentially due to its impact on improving the pulsating effect and decreasing the mass effect of aneurysms.[5,6] Lee et al. demonstrated successful flow diversion for 87 cases of ICA aneurysms <3 mm in diameter; 72% of cases achieved delayed washout or CO of the aneurysms immediately after treatment, and 93% achieved CO in the midterm follow-up.[7] This suggests that FD use is optimal for decreasing in-flow, leading to pulsating and mass effects for extremely small aneurysms. In the present case, neurological symptoms dramatically improved both consciously and objectively, with no changes in the aneurysm observed on DSA immediately after stenting.
Due to the comparatively small size and atypical symptoms of the aneurysm, the challenges encountered in this case primarily involved determining the suitability and timing of the therapeutic intervention. Most aneurysms that cause oculomotor palsy are typically large and accompanied by pupil symptoms.[8] Moreover, in our country, FDs are not typically used for such small CCAs. Consequently, it was imperative to carefully evaluate alternative diagnoses and consider the suitability of FDs. In the present case, the 4-mm CCA partly compressed the oculomotor nerve within the cavernous sinus from inside and below, leading to pupil-sparing oculomotor palsy. In the cavernous sinus, pupillary motor fibers of the oculomotor nerve are distributed in a complex and diffuse manner, whereas they run on the rostral surface in the intracranial segment.[8,9] Considering that early treatment of symptomatic aneurysms results in improved neurological outcomes,[10] we opted for early intervention and observed a favorable outcome.
Steroid administration before flow diversion may limit the assessment of its effectiveness. However, as previously mentioned, meticulous evaluation of the appropriateness and timing of flow diversion, while ruling out other potential causes, especially the relatively common Tolosa–Hunt syndrome, was crucial.[1] Conversely, antiplatelet therapy was initiated >7 days before stenting. Consequently, we initiated steroid and antiplatelet therapy simultaneously for diagnostic purposes, limiting our evaluation of the effectiveness of FDs. Nevertheless, the observation that neurological symptoms improved immediately following stenting, rather than in response to steroid therapy, suggests the effectiveness of flow diversion.
CONCLUSION
We successfully treated a case of small CCA with oculomotor palsy using early intervention with an FD, suggesting the effectiveness of this approach in managing small CCAs that cause neurological symptoms. Further, data are required to confirm the optimal nature of FDs.
Ethical approval
The research/study was approved by the Institutional Review Board at The Ethics Committee of Itabashi Chuo Medical Center, number 20230613, dated June 13, 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- A comparison of benign and inflammatory manifestations of Tolosa-Hunt syndrome. Cephalalgia. 2013;33:842-52.
- [CrossRef] [PubMed] [Google Scholar]
- Safety and effectiveness of the pipeline flex embolization device with shield technology for the treatment of intracranial aneurysms: Midterm results from a multicenter study. Neurosurgery. 2020;87:104-11.
- [CrossRef] [PubMed] [Google Scholar]
- Extending the indications of flow diversion to small, unruptured, saccular aneurysms of the anterior circulation. Stroke. 2014;45:54-8.
- [CrossRef] [PubMed] [Google Scholar]
- Cavernous carotid aneurysms in the era of flow diversion: A need to revisit treatment paradigms. AJNR Am J Neuroradiol. 2014;35:2334-40.
- [CrossRef] [PubMed] [Google Scholar]
- Flow diversion versus conventional treatment for carotid cavernous aneurysms. Stroke. 2014;45:2656-61.
- [CrossRef] [PubMed] [Google Scholar]
- Innovations in endovascular treatment strategies for large carotid cavernous aneurysms-the safety and efficacy of a flow diverter. J Stroke Cerebrovasc Dis. 2017;26:1071-80.
- [CrossRef] [PubMed] [Google Scholar]
- Flow diverter manages very small aneurysm of the internal carotid artery. J Chin Med Assoc. 2022;85:754-8.
- [CrossRef] [PubMed] [Google Scholar]
- Internal carotid artery aneurysm with incomplete isolated oculomotor nerve palsy: A case report. J Med Case Rep. 2023;17:77.
- [CrossRef] [PubMed] [Google Scholar]
- The pupillo-constrictor pathway and the nerves to the ocular muscles in man. Brain. 1946;69:301-9.
- [CrossRef] [PubMed] [Google Scholar]
- Small unruptured cerebral aneurysms presenting with oculomotor nerve palsy. Neurosurgery. 2003;52:553-7. discussion 556-7
- [CrossRef] [PubMed] [Google Scholar]






