Translate this page into:
Staged embolization of a double arteriovenous malformation in a pediatric patient: A case report

*Corresponding author: Arya Shariat, Department of Pediatrics, Kaiser LAMC, Los Angeles, California, United States. arya.shariat@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shariat A, Feng L. Staged embolization of a double arteriovenous malformation in a pediatric patient: A case report. Am J Interv Radiol 2023;7:14.
Abstract
Arteriovenous malformations (AVMs) are a rare vascular pathology of the central nervous system in pediatric patients; however, they are the most common cause of intracranial hemorrhage in this age group. Here, we describe a case of a 5-year-old female found to have a right double AVM with multiple enlarged feeding vessels. We performed a staged embolization, over three sessions, to achieve complete embolization of the AVM. Post-embolization angiography confirmed complete obliteration of shunting.
Keywords
Angiogram
Arteriovenous fistula
Arteriovenous malformation
Coil embolization
Pediatrics
INTRODUCTION
Arteriovenous malformations (AVMs) are relatively rare vascular lesions in the pediatric population but are associated with an increased risk of complications. They have a reported incidence of 1.3/100,000 patients/year with about 12–21% of them affecting children.[1] Children commonly present with spontaneous intraparenchymal hemorrhage, with an estimated overall yearly risk of hemorrhage from untreated AVMs ranging between 2% and 4%, a higher likelihood than in adults.[2] Diagnostic imaging techniques such as computer tomography (CT), magnetic resonance imaging (MRI), and magnetic resonance angiography (MRA) are crucial for diagnosis, localization, and treatment planning. The primary goal of AVM treatment is to achieve complete angiographic occlusion while minimizing neurological sequelae. Although surgical resection is the preferred method, complications such as hemorrhage and brain tissue damage necessitate considering adjunctive therapies like endovascular embolization, especially for high-grade AVMs.[3] Endovascular embolization has demonstrated feasibility and safety in managing pediatric AVMs and is expected to advance further with improved technology, enhancing its role as an adjunctive treatment option in this population.[2,3] We present a case report detailing a successful complete occlusion of a double AVM in a 5-year-old female through staged embolization, with minimal complications.
CASE REPORT
A 5-year-old female presented with a 2 day history of headaches accompanied by photophobia, nausea, fatigue, and vomiting. Due to concerns regarding worsening headaches with exertion, a CT was performed, revealing a complex 2.7 × 2.9 × 2.3 cm and 2.0 × 1.8 × 2.1 cm right hemispheric extra-axial vascular mass [Figure 1]. Subsequent MRI showed an AVM in the right superior temporal-toparietal region, while MRA revealed the presence of multiple enlarged feeding arteries originating from the cerebral arteries and draining veins measuring up to 29 mm in diameter. She was placed on keppra for seizure prophylaxis while the case was discussed with an interdisciplinary team consisting of pediatric neurosurgery, pediatric neurology, and interventional radiology.
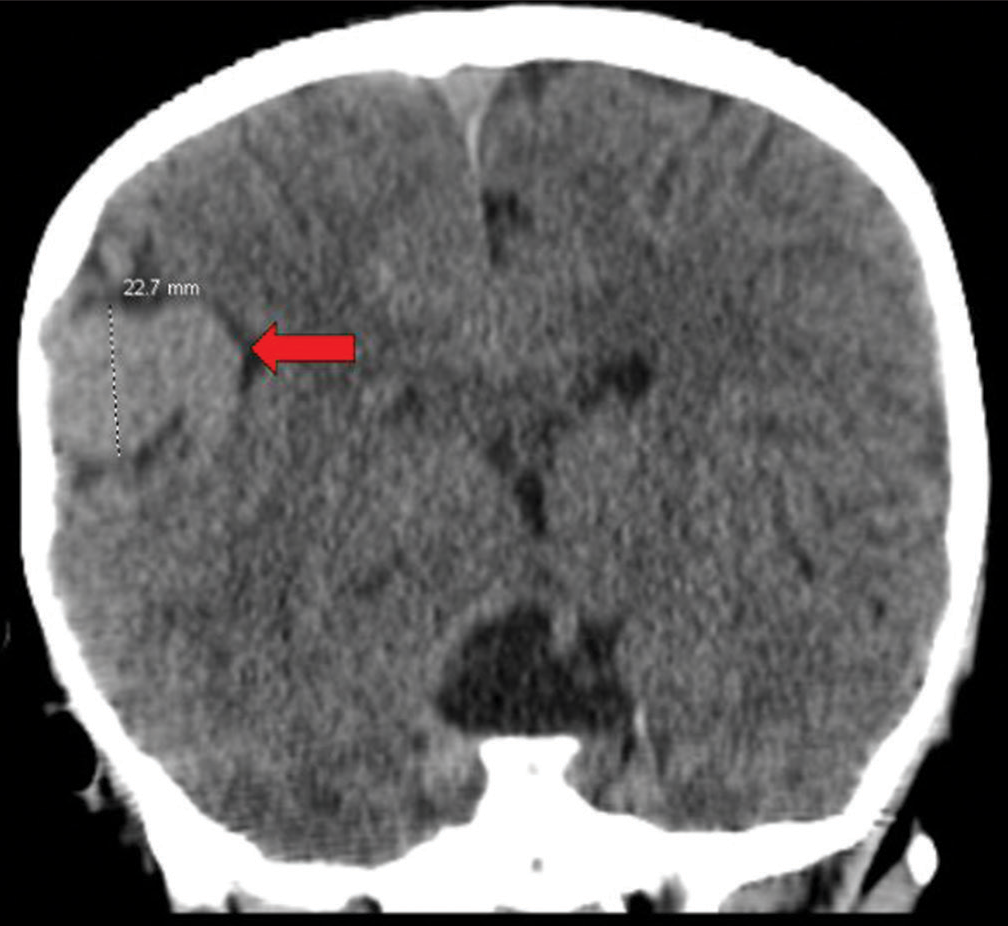
- A 5-year-old female presented with headache found to have two direct arteriovenous fistulas along the right temporal parietal lobe. Non-contrast showing complex, ill-defined extra-axial masses measuring 2.7 × 2.9 × 2.3 cm and 2.0 × 1.8 × 2.1 cm (red arrow).
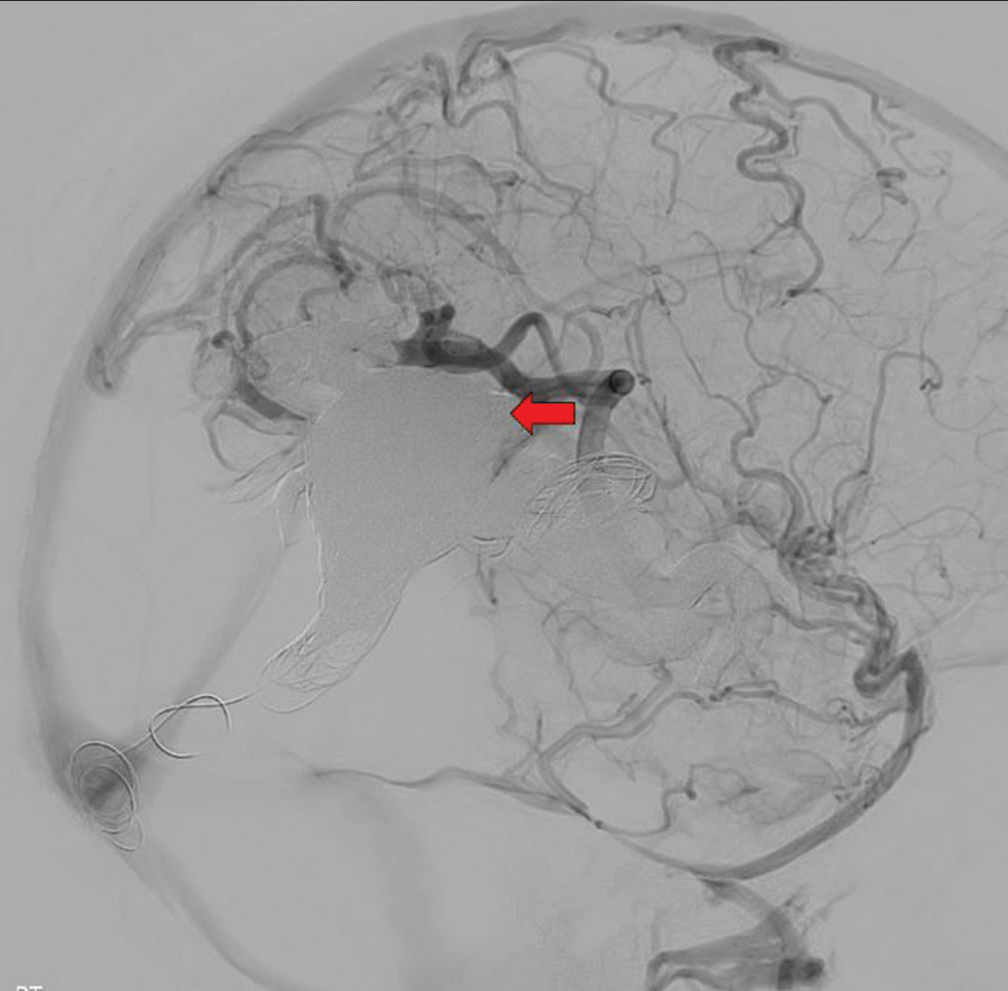
A cerebral angiogram revealed two AVMs along the right temporal-parietal lobe, supplied by dilated branches of the right middle cerebral artery (MCA), with superficial venous drainage leading to the right transverse sinus [Figure 2]. The more posterior lesion had a 3.5 × 2.5 cm venous pouch, supplied by dilated branches of the right coronary arteries. An abundant collateral supply to bilateral vertebral arteries and internal carotid arteries was observed from the external carotid arteries. The decision was made to perform a staged embolization of the AVM.
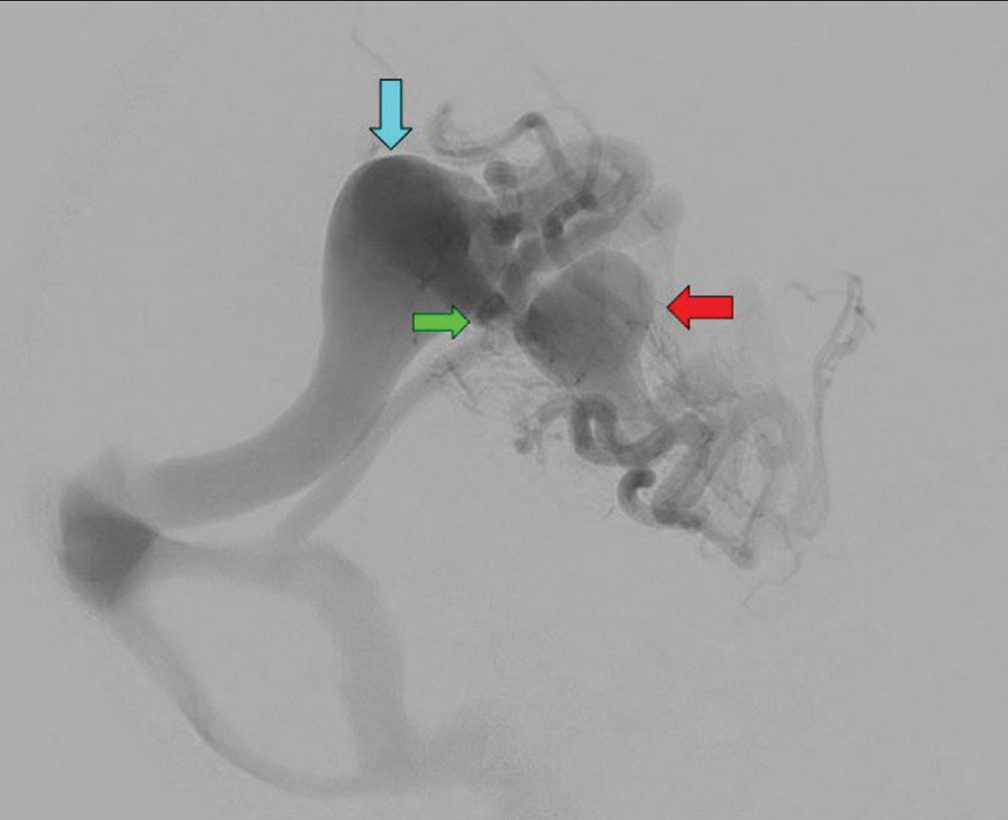
- A 5-year-old female presented with headaches found to have two direct arteriovenous fistulas along the right temporal parietal lobe. Digital subtraction angiogram showing two direct arteriovenous fistulas in the right temporal parietal lobe. The more anterior lesion has a 2 × 2 cm venous pouch (red arrow), supplied by dilated temporal branches of the right middle cerebral artery (MCA) and right posterior cerebral artery (PCA). This lesion has a unique draining vein but is also connected to the venous pouch of the more posterior lesion (green arrow). The more posterior lesion has a 3.5 × 2.5 cm venous pouch (blue arrow), supplied by dilated parietal branches of the right MCA and right PCA.
A 1.5 cm Apollo microcatheter (Medtronic, Minneapolis, MN USA) was advanced from the right common femoral artery toward the right temporal AVM. To reduce flow, i-ED coils (Kaneka Corp, Osaka City, Tokyo, Japan) sized 0.012 in × 20 mm × 50 cm and 4–10 mm × 30 cm were placed into the venous pouch. In addition, two iED coils sized 4 mm × 10 cm and 3.5 mm × 8 cm were introduced into the main feeding arteries. Embolization of the feeding arteries was performed using Onyx (Medtronic, Minneapolis, MN USA). Digital subtraction angiogram (DSA) showed occlusion of the right temporal AVM, while the right parietal AVM remained unaffected [Figure 3]. She presented to the emergency department after the embolization with complaints of headache and vomiting. She tested positive for human coronavirus, coinciding with the upper respiratory symptoms.
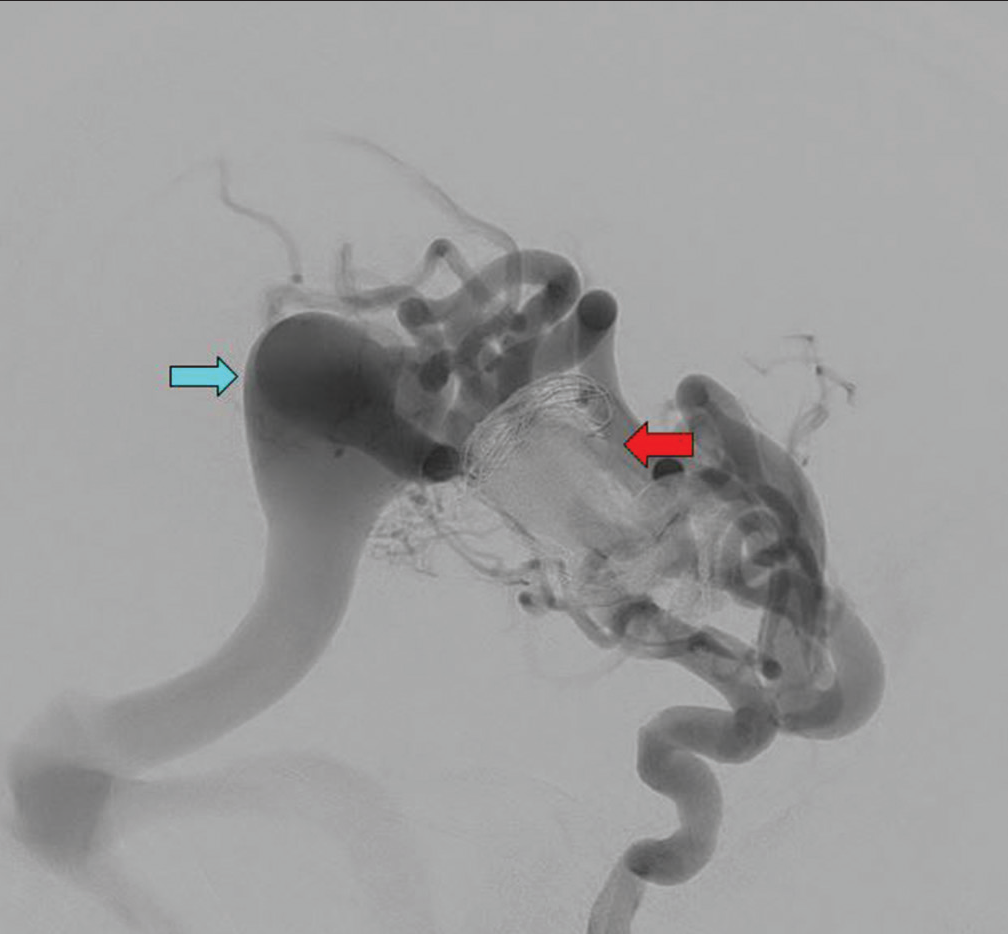
- A 5-year-old female presented with headaches found to have two direct arteriovenous (AV) fistulas along the right temporal parietal lobe. Digital subtraction angiogram showing evidence of successful occlusion of the right temporal AV fistula with coils and Onyx (red arrow). Unperturbed right parietal AV fistula (blue arrow).
One month after the initial embolization, she underwent the second stage of embolization. Three vessels were identified supplying the right parietal AVM, with the largest being the right posterior temporal branch of the right MCA. A Headway Duo microcatheter (Terumo-MicroVention, Shibuya-ku, Tokyo, Japan) was advanced into the larger feeding artery, and an unsuccessful attempt was made to tangle two coils together using the two-catheter technique with different-sized coils. Instead, a 6 × 15 mm Eclipse balloon catheter (Balt Medical, Irvine, California, USA) was advanced into the largest feeding artery along with an Apollo catheter, and while the balloon inflated and flow was slowed, an i-ED 4 mm × 10 cm coil was deployed into the artery. In addition, a 6 mm × 20 cm Wallaby coil (Wallaby Medical, Laguna Hills, California, USA) was deployed downstream from the i-ED coil to assist in anchoring it. The large feeding artery was then embolized using Onyx with complete occlusion of the feeding artery and the refluxing distal collateral vessels [Figure 4]. Following the second embolization, she presented to the ED with a headache and vomiting. She did not have any neurological deficits during the admission, and the MRI suggested pansinusitis without evidence of hemorrhage or infarct.
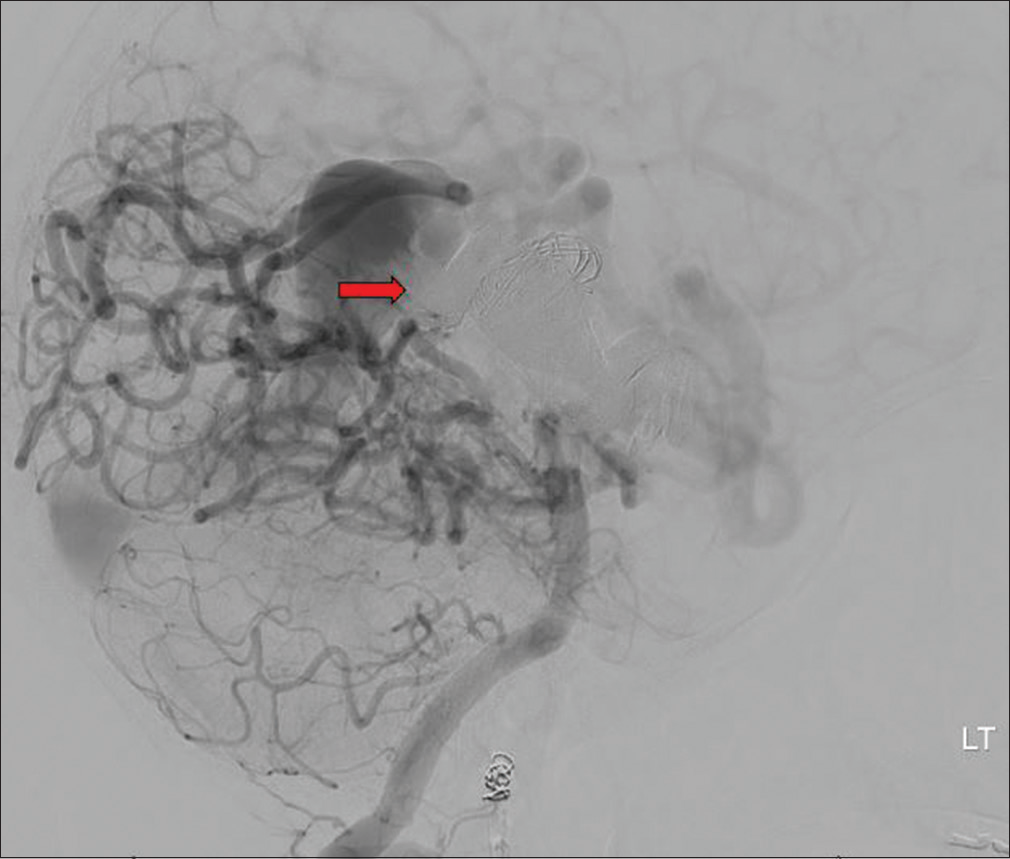
- A 5-year-old female presented with headaches found to have two direct arteriovenous fistulas along the right temporal parietal lobe. Digital subtraction angiogram showing successful balloon-assisted Onyx embolization of the largest feeding artery to the right parietal arteriovenous malformation (red arrow) with marked reduction of stealing phenomenon and better flow to the right middle cerebral artery cortical branches.
The third and final stage of embolization was performed using a combination of transvenous and transarterial approaches. An Echelon-10 microcatheter (Medtronic, Minneapolis, MN USA) was advanced through a left venous access point and navigated to the venous pouch of the fistula. Subsequently, a 6 × 15 mm Eclipse balloon catheter was inserted through a right arterial access point and positioned in the right M2 segment. A 1.5 cm Apollo microcatheter was placed in the feeding artery of the venous pouch over a 008 hybrid wire (Balt Medical, Irvine, California, USA). To impede arteriovenous (AV) shunting, the Eclipse balloon was inflated in the main M2 branch of the right MCA, effectively obstructing the MCA feeding arteries to the fistula. A Target XL 360 Standard 24 mm × 50 cm coil (Stryker Corp, Kalamazoo, Michigan, USA), was deployed within the venous pouch, establishing a stable framework. In addition, two Wallaby 25 mm × 60 cm coils, two Wallaby 22 mm ×50 cm coils, five Axium 3D 25 mm × 50 cm coils (Medtronic, Minneapolis, MN USA), and another two Target XL 360 Standard coils were introduced to reinforce the venous pouch. Due to difficult flow within the large venous pouch, part of the coil was allowed to flow to the junction of the draining vein and right transverse sinus to anchor it. Onyx was injected into the venous pouch eventually leading to the formation of an anterior cast with reflux into other collateral feeding arteries. DSA demonstrated complete occlusion of the right temporal fistula [Figures 5 and 6].
- A 5-year-old female presented with headaches found to have two direct arteriovenous (AV) fistulas along the right temporal parietal lobe. Digital subtraction angiogram showing successful transvenous and transarterial embolization of right temporal arteriovenous fistula with complete obliteration of AV shunting (red arrow) and improved cortical flow to the right middle cerebral artery territory.
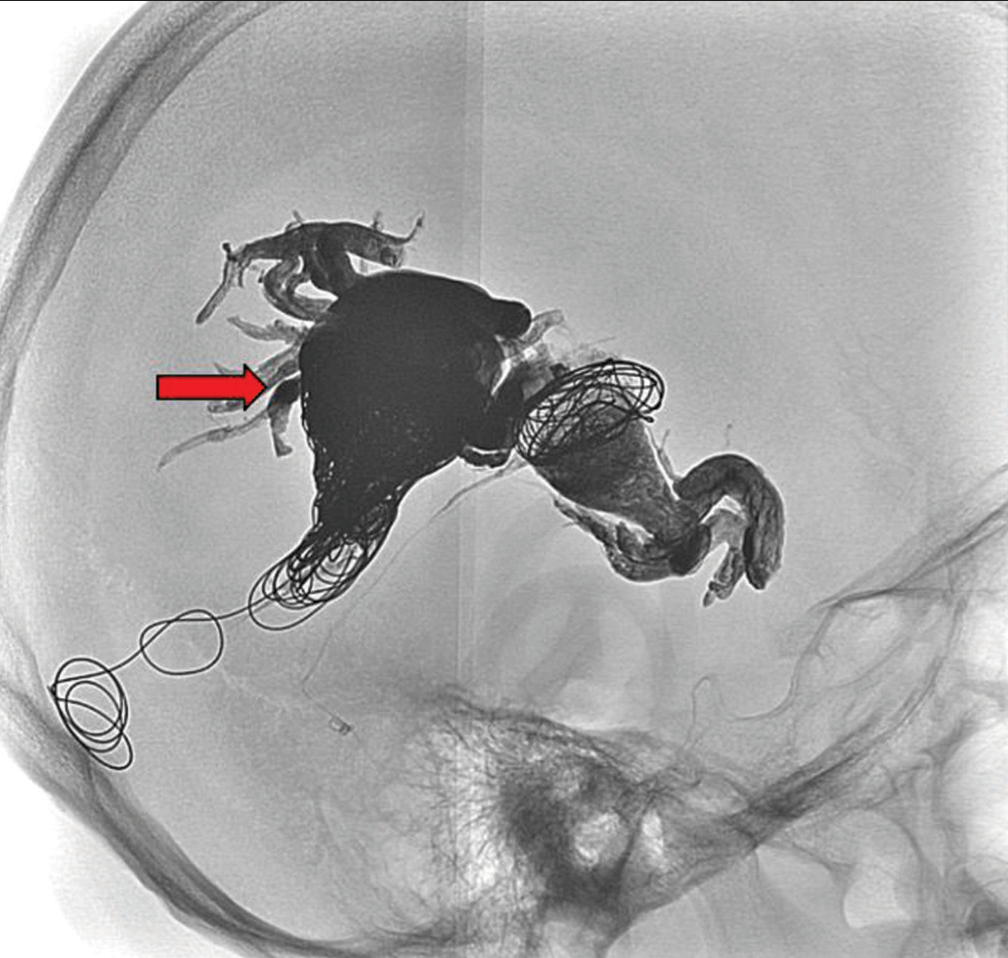
- A 5-year-old female presented with headaches found to have two direct arteriovenous (AV) fistulas along the right temporal parietal lobe. Digital subtraction angiogram showing successful transvenous and transarterial embolization of the right temporal arteriovenous fistula with complete obliteration of AV shunting and improved cortical flow to the right middle cerebral artery territory (image of complete staged occlusion – red arrow).
At the 6-month follow-up, the patient continued to show improvement in her headache symptoms. There were no reported seizures, weakness, numbness, or speech problems during the staged correction process.
In conclusion, successful embolization of the right temporal-parietal double AVM, resulting in complete obliteration of AV shunting and improved blood flow.
DISCUSSION
We present a case involving a pediatric patient who underwent staged embolization over a 6-month period for an AVM with multiple feeding vessels. In patients suspected of having an AVM, CT is the recommended initial imaging modality to assess for hemorrhage. When considering treatment options, lesions can be categorized into low-grade (I–III) and high-grade (IV–V) lesions based on the size of the nidus, the eloquence of adjacent brain tissue, and the pattern of venous drainage.[2] Treatment options vary depending on whether an AVM is ruptured or unruptured, as ruptured cases carry a higher risk of recurrent hemorrhage and increased neurological morbidity, often necessitating treatment. Since AVMs tend to present earlier in children, a higher lifetime hemorrhage risk must be taken into account when considering treatment. The annual risk of rupture of untreated AVMs in children is 4.4–5.5%.[4]
The gold standard for the treatment of intracranial AVMs is surgery; however, the complication rate associated with surgical intervention of unruptured AVMs is increased in patients with non-hemorrhagic presentation, large AVM diameter, involvement of deep venous drainage, or those located in eloquent brain regions.[5] These lesions are commonly treated with either embolization, which can fully embolize the AVM or reduce the flow before surgery, or with stereotactic radiosurgery (SRS). After embolization therapy, complete radiographic resolution is estimated to occur in 10–40% of AVMs, while SRS has an estimated obliteration rate of 60–70%.[4] Common complications from endovascular embolization include vessel perforation, puncture site hematoma, retrograde embolization of normal arteries, or material-related complications such as pulmonary edema secondary to Onyx in the pulmonary artery.[2] In the pediatric population, treatment decisions should be individualized based on the specific characteristics of the AVM and the patient’s clinical situation.
Multiple AVMs are relatively rare with only a few reported cases.[6,7] Patients with multiple AVMs face an elevated risk of various complications, including hemorrhages, neurological issues, venous infarctions, and cortical venous reflux.[7] The etiology of multiple AVMs can be categorized into congenital and acquired causes. Congenital factors include conditions such as Rendu-Osler-Weber syndrome, hereditary hemorrhagic telangiectasia, and Wyburn-Mason syndrome.[8] Acquired multiple AVMs can arise due to several mechanisms, including angiogenesis around an existing AVM, as pial shunts associated with dural AVM, or as secondary consequences to sinus thrombosis, head trauma, surgical procedures, hormonal fluctuations, or infection.[6] Ultimately, leading to increased blood flow into the dural sinuses.
Multiple AVMs are associated with unfavorable clinical outcomes, especially when left untreated.[9] Embolization plays a crucial role by providing endovascular ligation, facilitating safe and effective resection, reducing intraoperative blood loss, and minimizing the risk of normal perfusion pressure breakthrough.[3] Moreover, staged and repeated embolization yielded good results in 70% of patients with multiple AVMs.[7] In cases where accessing deep arterial feeders surgically is challenging, embolization offers viable treatment options.
CONCLUSION
This case report describes a staged approach to embolization of a right temporal-parietal double AVM, resulting in complete obliteration of the AVMs and minimal complications observed at the 6-month follow-up. Radiologists should be aware of the strengths and limitations of various imaging modalities when assessing AVMs, as well as the different treatment options available.
Declaration of patient consent
Patient’s consent was not required as patients identity was not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Children with arteriovenous malformations of the central nervous system: A retrospective study of 12 pediatric cases from a single tertiary center in Slovenia. Med Sci Monit. 2022;28:e936240.
- [CrossRef] [PubMed] [Google Scholar]
- Arteriovenous malformations in the pediatric population: Review of the existing literature. Interv Neurol. 2016;5:218-25.
- [CrossRef] [PubMed] [Google Scholar]
- Endovascular treatment in the multimodality management of brain arteriovenous malformations: Report of the society of neurointerventional surgery standards and Guidelines Committee. J Neurointerv Surg. 2022;14:1118-24.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric intracranial arteriovenous malformations: A single-center experience. J Neurosurg Pediatr. 2020;25:151-8.
- [CrossRef] [Google Scholar]
- Determinants of staged endovascular and surgical treatment outcome of brain arteriovenous malformations. Stroke. 2005;36:2431-5.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple cerebral arteriovenous shunts in children: Report of 13 cases. Childs Nerv Syst. 1992;8:437-44.
- [CrossRef] [PubMed] [Google Scholar]
- Endovascular management of multiple intracranial dural arteriovenous fistulas. J Neuroradiol. 2019;46:390-7.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple cerebral arteriovenous malformations (AVMs) Neuroradiology. 1990;32:207-10.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and angiographic characteristics of multiple dural arteriovenous shunts. Am J Neuroradiol. 2012;33:1691-5.
- [CrossRef] [PubMed] [Google Scholar]






