Translate this page into:
Insufflation of the gastric remnant from a transduodenal approach facilitates percutaneous gastrostomy tube placement in a post Roux-en-Y patient

*Corresponding author: Michael Curtis Jundt, Department of Radiology, Mayo Clinic, Rochester, United States. jundt.michael@mayo.edu
-
Received: ,
Accepted: ,
How to cite this article: Yousif P, Thompson SM, Jundt MC. Insufflation of the gastric remnant from a transduodenal approach facilitates percutaneous gastrostomy tube placement in a post Roux-en-Y patient. Am J Interv Radiol. 2025;9:4. doi: 10.25259/AJIR_62_2024
Abstract
Percutaneous gastrostomy tube insertion in post Roux-en-Y patients can be challenging due to decompression of the excluded stomach and its discontinuity with the proximal enteric tract. Presented here is a 65-year-old woman status post Roux-en-Y gastric bypass who required gastrostomy tube placement for enteral feeding. The remnant stomach collapsed, and direct percutaneous gastric access was not possible for insufflation. To facilitate insufflation, computed tomography (CT) was used to access the duodenal bulb. This duodenal access was used to insufflate the stomach in a retrograde fashion which created a safe percutaneous window for gastrostomy tube placement into the remnant stomach. The technique described in this study can be a useful tool in patients with difficult to access remnant stomachs. Utilizing either direct or transhepatic access to the duodenum with ultrasound or CT guidance for remnant stomach insufflation can facilitate gastrostomy tube placement in challenging cases.
Keywords
Enteral nutrition
fluoroscopy
gastric bypass
multidetector computed tomography
tubes gastro
INTRODUCTION
Roux-En-Y gastric bypass is considered the gold standard for the surgical management of medically complicated obesity. The procedure results in a restrictive-malabsorptive state through the creation of a gastric pouch, pancreaticobiliary limb, gastrojejunostomy, and jejunojejunostomy. This anatomy allows ingested food to bypass the duodenum and most of the stomach, known as the excluded or remnant stomach.[1] Following Roux-en-Y gastric bypass, patients may require access to the excluded stomach for enteral feeding or decompression. A radiologically inserted gastrostomy (RIG) is one method of placing a percutaneous gastrostomy tube into the excluded stomach. This method requires distension of the gastric remnant to create a safe percutaneous window for subsequent gastrostomy tube placement.[2] Access to the gastric remnant can be challenging, especially when it is decompressed. Computed tomography (CT) may help facilitate access to the excluded stomach in cases where the excluded stomach is not visible by either ultrasound or fluoroscopy or when indirect routes are required (such as transhepatic). Technical failures can occur when the remnant stomach cannot be accessed, even with CT guidance.[2]
Here, we present a case of a patient with a history of Roux-en-Y gastric bypass who required placement of a percutaneous gastrostomy tube for feeding following repair of an esophageal perforation. Access into the excluded stomach was gained through an indirect transduodenal approach after direct access could not be achieved due to gastric remnant decompression.
CASE REPORT
The patient is a 65-year-old female with a history of atrial fibrillation (not on anticoagulation), hypertension, and Rouxen-Y gastric bypass performed 20 years ago for weight loss. Nine years ago, the patient underwent C5–C6 anterior cervical discectomy and fusion for cervical radiculopathy. Hardware infection necessitated a recent revision surgery with hardware explantation. The revision was complicated by an esophageal perforation for which a repair was promptly undertaken. Following the repair, the patient was made nil per os and required enteral access for feeding. She was subsequently referred to interventional radiology for percutaneous gastrostomy tube placement into the remnant stomach.
Pre-procedure CT demonstrated a decompressed gastric remnant with a possible small percutaneous window [Figure 1]. The procedure was performed in a hybrid procedural suite containing ultrasound, fluoroscopy, and CT. The patient was placed under general anesthesia. A CT of the upper abdomen was performed to identify a percutaneous window to the decompressed remnant stomach for insufflation. Once a window was identified and following sterile preparation and injection of 1% lidocaine for local anesthesia, a 15 cm length, 22-gauge Chiba needle (Cook Medical, Bloomington, Indiana) was advanced into the remnant stomach. An 80 cm, 0.018” Nitrex guidewire (Medtronic, Minneapolis, MN) was advanced through the needle, but the wire would not form in the lumen of the collapsed remnant stomach.

- A 65-year-old female with esophageal perforation and a remote history of gastric bypass requiring enteral access for feeding. Non-contrast enhanced computed tomography of the upper abdomen performed in the procedure suite for planning purposes demonstrates the decompressed gastric remnant (black arrow).
Two 22-gauge needles were then advanced under CT guidance into the air-filled duodenal bulb. One of the 22-gauge needles was used to pin the mobile duodenum in place while the other needle was used to access the duodenal lumen [Figure 2]. Water soluble contrast was injected through the needle to document position in the duodenum. The 0.018” Nitrex wire was advanced into the second portion of the duodenum. An AccuStick II Introducer System (Boston Scientific, Marlborough, Massachusetts) was used to covert the tract to an 0.035” system. Through the AccuStick II Introducer sheath, a 4 french Kumpe catheter (Angiodynamics, Latham, New York) and 0.035” GLIDEWIRE standard (Terumo Interventional Systems, Tokyo, Japan) were negotiated retrograde across the pylorus into the remnant gastric lumen. From this access, the excluded stomach was then insufflated with room air. The 22-gauge needle was then inserted into the distended excluded stomach lumen followed by placement of the 0.018” Nitrex, conversion of the tract with the AccuStick II Introducer System, and placement of a 0.035” Nitrex wire (Medtronic, Minneapolis, MN). Over the guidewire, a coaxial angioplasty balloon technique without gastropexy, as described elsewhere,[3] was used to place a 16-French Kimberly-Clark MIC gastrostomy tube (Avanos Medical, Alpharetta, GA) into the remnant stomach [Figure 3a]. The retention balloon was filled with 5 mL of dilute contrast and the external disc was secured down to the skin. Final gastrostomy tube position was confirmed with a final contrast injection under fluoroscopy [Figure 3b]. Enteral feeds through the gastrostomy tube were initiated the following day and were well tolerated.

- A 65-year-old female with esophageal perforation and a remote history of gastric bypass requiring enteral access for feeding. Non-contrast-enhanced intraprocedural computed tomography of the upper abdomen. Two 22-gauge needles were used to access the duodenal bulb, which was distended with fluid and air. The medial needle was used to pin the mobile duodenum, and the lateral needle was used to access the duodenal lumen.
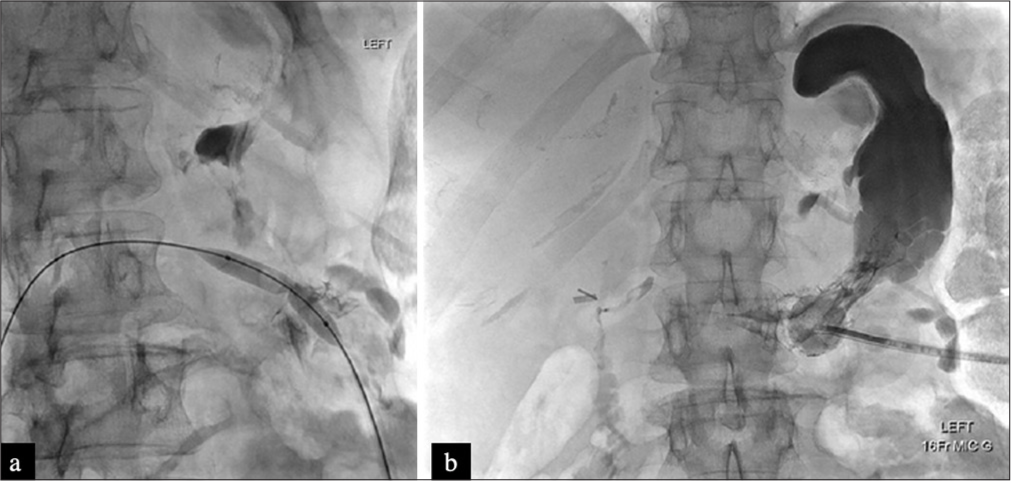
- A 65-year-old female with esophageal perforation and a remote history of gastric bypass requiring enteral access for feeding. (a) Fluoroscopic image demonstrates the over-the-wire coaxial balloon angioplasty technique for gastropexy and subsequent percutaneous gastrostomy tube placement. (b) Final fluoroscopic image demonstrates gastrostomy tube position in the gastric remnant.
DISCUSSION
Gastrostomy tube placement in patients with a history of Roux-en-Y gastric bypass can be challenging. While surgical gastrostomy is the conventional approach, this technique may be complicated by post-operative adhesions or significantly altered anatomy from prior surgeries.[4,5] The use of endoscopic ultrasound (EUS)-guidance for excluded gastric remnant access has been described, but this technique requires experience with EUS and two operators.[6] RIG tube placement in excluded gastric remnants has become both more feasible and common over the past two decades as experience using a combination of ultrasound, CT, and fluoroscopy has evolved.[2,7]
As with RIG tube placement in patients with standard gastric anatomy, the percutaneous placement of a gastrostomy tube in Roux-en-Y patients requires a percutaneous window to the excluded gastric remnant without intervening bowel or liver. Distension of the gastric remnant can be safely accomplished through transhepatic or transenteric routes using small (21- or 22-gauge) needles.[2] Once the remnant is distended, a safe window for percutaneous gastric remnant gastrostomy can be chosen. While uncommon, access of the remnant with even a small needle may not be possible if the remnant is completely collapsed.
Here, we describe a technique for accessing decompressed gastric remnants from a transduodenal approach to facilitate insufflation of the remnant stomach for subsequent gastrostomy tube placement. In our case, the gastric remnant was collapsed and the coapted gastric walls would not accommodate a wire. The first portion of the duodenum was dilated, amenable to access, and facilitated distension of the remnant. To the best of our knowledge, access of the remnant from a retrograde transduodenal approach has not been reported before, but percutaneous duodenal access has been reported in the gastroenterology literature. Percutaneous duodenal access during percutaneous cholecystoenteric anastomosis creation was shown to be safe without any adverse events in a study including 14 patients.[8]
This technique may not be possible if the duodenum is decompressed or if there is not a safe window to access the duodenum directly. This approach also relies on the use of CT, which may not be available to all proceduralists. There are some potential complications which could arise from this procedure, including duodenal perforation and bleeding. The complication rate regarding percutaneous duodenal access is not well known due to the paucity of literature; the complication rate for percutaneous jejunostomy tube placement is about 10–11%, but this is involves placement of a larger bore catheter directly into the jejunum.[9]
CONCLUSION
For gastrostomy tube placement in Roux-en-Y patients with difficult to access gastric remnants, transduodenal insufflation can be considered. This technique provides a less invasive option for patients who would otherwise need to undergo either laparoscopic or open surgery.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Roux-en-Y gastric bypass, sleeve gastrostomy, or one-anastomosis gastric bypass? A systematic review and meta-analysis of randomized-controlled trials. Obesity (Silver Spring). 2022;30:614-27.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous gastric remnant gastrostomy following Roux-en-Y gastric bypass surgery: A single tertiary center's 13-year experience. Abdom Radiol (NY). 2018;43:1464-71.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous radiologic gastrostomy catheter placement without gastropexy: A coaxial balloon technique and evaluation of safety and efficacy. Abdom Radiol. 2016;41:2227-32.
- [CrossRef] [PubMed] [Google Scholar]
- Guidelines for gastrostomy tube placement and enteral nutrition in patients with severe, refractory hypoglycemia after gastric bypass. Surg Obes Relat Dis. 2021;17:456-65.
- [CrossRef] [PubMed] [Google Scholar]
- Laparoscopic insertion of a percutaneous gastrostomy prevented malnutrition in a patient with previous Roux-en-Y gastric bypass. Obes Facts. 2022;15:458-62.
- [CrossRef] [PubMed] [Google Scholar]
- A pilot study of percutaneous cholecystoenteric anastomosis: A new option for high-risk patients with symptomatic gallstones. J Vasc Interv Radiol. 2024;35:74-9.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous gastrostomy of the excluded gastric segment after Roux-en-Y gastric bypass surgery. J Vasc Interv Radiol. 2007;18:914-9.
- [CrossRef] [PubMed] [Google Scholar]
- EUS-assisted, fluoroscopically guided gastrostomy tube placement in patients with Roux-en-Y gastric bypass: A novel technique for access to the gastric remnant. Gastrointest Endosc. 2011;74:677-82.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous jejunostomy. Semin Intervent Radiol. 2004;21:199-204.
- [CrossRef] [PubMed] [Google Scholar]






