Translate this page into:
External validation of a quantitative model to guide patient selection for placement of an optional or permanent inferior vena ca va filter

*Corresponding author: Aliaksei Salei, Department of Radiology, University of Alabama at Birmingham, Birmingham, Alabama, United States. asalei@uabmc.edu
-
Received: ,
Accepted: ,
How to cite this article: Song E, Salei A, Li Y, Brown SR, El Khudari H, Gunn AJ. External validation of a quantitative model to guide patient selection for placement of an optional or permanent inferior vena cava filter. Am J Interv Radiol. 2024;8:18. doi: 10.25259/AJI R_32_2024
Abstract
Objectives:
The objective of this study was to validate a previously published quantitative model that predicts the likelihood of an optional inferior vena cava filter (IVCF) being kept as a permanent device in a different patient population.
Material and Methods:
An institutional database of IVCF patients from 2016 to 2018 was reviewed. As in the published reference, if a retrieval was attempted, the IVCF was categorized as “removed;” if no attempt was performed, the filter was categorized as “kept permanent.” Patient parameters, such as age, sex, history of venous thromboembolism, presence of neurologic disease, presence of malignancy, as well as indications for IVCF placement were analyzed. The previously published formula was applied to analyze its ability to predict the likelihood of an optional IVCF being kept permanently in a new, external population.
Results:
A total of 270 patients were identified. Seventy-one filters were “removed” and 199 were “kept permanent.” Advanced age (odds ratio [OR] 1.05; 95% confidence interval [CI] 1.03–1.07) and presence of malignancy (OR 2.55; 95% CI 1.29–5.07) were the factors associated with the IVCF being “kept permanent” versus “removed.” None of the other parameters was statistically significant. The receiver operating characteristic curve yielded the area under the curve of 0.66, compared to the previously published value of 0.8. The sensitivity and specificity of the model were 64.3% and 62.0%, respectively.
Conclusion:
Advanced age and presence of malignancy were associated with optional IVCFs being kept as permanent devices. However, the previously published formula did not yield an accurate quantitative prediction in this external patient population.
Keywords
inferior vena cava filter
venous thromboembolism
pulmonary embolism
permanent filters
INTRODUCTION
Inferior vena cava filter (IVCF) placement has been performed in various clinical situations in patients with venous thromboembolism (VTE).[1] In addition, filtration was previously recommended prophylactically in patients with high risk of VTE,[2-4] although the majority of current guidelines discourage prophylactic use.[1,5,6] The Food and Drug Administration (FDA) approval of optional, or retrievable, filters in 2003 contributed to the increase in use of IVCFs in the US from 2000 to 2009.[7] Growing awareness of potential risks associated with IVCF placement resulted in 2010 and 2014 FDA warnings encouraging physicians to ensure proper follow-up for patients who have received an optional IVCF.[8,9] Over the past decade, multiple reports were published illustrating the efficacy of dedicated programs in improving filter retrieval rates. Despite that, a significant proportion of filters remain unretrieved, with reported retrieval rates ranging from 28% to 60%.[10-14] A significant proportion of patients either die during the follow-up period or their filters are deemed permanent on follow-up.[14] This subgroup of patients could benefit from placement of permanent IVCFs, which are associated with less reported complications,[15-17] less cost, and do not require dedicated follow-up.[17] In 2013, Eifler et al. published a study utilizing logistic regression analysis for modeling optional IVCF permanence, based on multiple patient parameters correlating to retrievability of these filters, and formulated an equation that would aid clinicians in the decision between placing an optional versus a permanent filter. The study yielded a c-statistic of the formula of 0.8, indicating a good predictive ability.[18] This formula has never been validated on an external patient population. Thus, our study aims to externally validate this quantitative model.
MATERIAL AND METHODS
The study was approved by the Institutional Review Board and was Health Insurance Portability and Accountability Act compliant. IVCF placement was performed in accordance with published guidelines.[3]
Patient selection
A dedicated IVCF retrieval program was initiated at our institution in July 2016. Medical records of consecutive patients who received IVCFs during 2 years after the program initiation, from July 2016 to June 2018, were retrospectively reviewed. All patients who received retrievable IVCF were included. Like the previously published report, all optional IVCFs were placed with an intent of future retrieval. Permanent filters placed in patients with limited life expectancy at the discretion of an interventional radiologist were excluded from this study.
Study design
As per the previously published report, if a retrieval of the optional IVCF was attempted, the IVCF was categorized as “removed;” If no attempt was performed, the IVCF was categorized as “kept permanent.” The outcomes of retrieval procedures were not accounted. The “kept permanent” category consisted of the filters that were “deemed permanent” (based on a documented decision to keep filter in place by a physician or a patient), “lost to follow-up,” or “expired” (if a patient died before assessment regarding filter retrieval). The structure of our institutional program and the decision process is consistent with that described by Eifler et al. The same patient parameters as in the reference publication were collected and analyzed, namely, age, sex, history of VTE, presence of neurologic disease, presence of active malignancy, as well as indications for IVCF placement utilizing the description of the categories based on the reference.[18]
Device description, placement, and removal
IVC filters were placed and retrieved by board certified or board eligible interventional radiologists. Four types of retrievable IVC filters were placed at our institution during the study period; including, Denali™ (Bard, Murray Hill, NJ), Celect™ (Cook, Bloomington, IN), Günther Tulip® (Cook), and Optease™ (Cordis, Hialeah, FL). The choice of filter type was based on operator preference or availability at the time of placement. Most filter retrievals were performed utilizing a standard snare technique. If retrieval with standard technique was not feasible, an advanced retrieval technique (typically utilizing loop snare or endobronchial forceps) was attempted during the same session.
Statistical analysis
The patient parameters between “removed” and “kept permanent” groups were compared utilizing a Chi-square test and two-group student t-test for categorical and continuous variables, respectively. Subsequently, we applied the univariate logistic regression analysis to our patient cohort to evaluate probability of retrieval. Odds ratios (ORs) and two-sided 95% confidence intervals (CIs) were estimated. A receiver operating characteristic curve for reference predicted probabilities (calculated by applying the formula in the reference[18]) was created. Sensitivity and specificity of model prediction were estimated using recursive operating curve analysis based on the largest Youden index. Analysis was performed using Statistical Analysis Software v9.4.
RESULTS
A total of 270 patients with removable IVCFs were identified during the study period. Seventy-one filters (26.3%) were categorized as “removed” and 199 (73.7%) were “kept permanent.” The patient parameters are summarized in Table 1. The age at placement was statistically significant, with the patients in “removed” category being younger in comparison to “kept permanent” (mean age 63.8 vs. 50.6 years; P < 0.001). A statistically higher proportion of patients with history of malignancy were in the “kept permanent” category in comparison to the “removed” category (34.2% vs. 16.9%; P = 0.0062). No other statistically significant differences were identified between the two groups.
| Retrieval Attempt | P-value | ||
|---|---|---|---|
| No (n=199) (%) | Yes (n=71) (%) | ||
| Age at placement | <0.0001 | ||
| Mean±SD | 62.9±14.3 | 51.7±15.3 | |
| Median | 63.8 | 50.6 | |
| Min–Max | 17.6–90.2 | 17.6–83.6 | |
| Sex | 0.92 | ||
| Female | 94 (47.24) | 34 (47.89) | |
| Male | 105 (52.76) | 37 (52.11) | |
| History of VTE | 0.32 | ||
| No | 6 (3.02) | 4 (5.63) | |
| Yes | 193 (96.98) | 67 (94.37) | |
| Presence of malignancy | 0.0062 | ||
| No | 131 (65.83) | 59 (83.10) | |
| Yes | 68 (34.17) | 12 (16.90) | |
| Presence of neurologic disease | 0.65 | ||
| No | 132 (66.33) | 45 (63.38) | |
| Yes | 67 (33.67) | 26 (36.62) | |
| Indication for filter placement | 0.5 | ||
| VTE/anticoagulation contraindication | 154 (77.39) | 56 (77.46) | |
| VTE/anticoagulation complication | 31 (15.58) | 7 (9.86) | |
| VTE/anticoagulation failure | 7 (3.52) | 4 (5.63) | |
| High-risk VTE | 1 (0.50) | 0 (0) | |
| Prophylaxis | 6 (3.02) | 4 (5.63) | |
SD: Standard deviation, VTE: Venous thromboembolism
The univariate logistic regression analysis of the parameters was subsequently performed. Given that only one patient with high risk VTE was present in the studied cohort, a logistic regression analysis was performed with exclusion of the high-risk VTE patients and summarized in Table 2. Of those, advanced age was associated with the IVCF being kept permanently versus retrieved (OR 1.05; 95% CI 1.03–1.07; P < 0.001) as well as the presence of malignancy (OR 2.55, 95% CI 1.29–5.07; P = 0.0075). None of the other parameters, including sex, history of VTE, presence of neurologic disease, indication for IVCF placement due to VTE/anti-coagulation complication, or indication for IVCF placement due to VTE/anti-coagulation failure was statistically significant.
| Unadjusted OR | 95% CI | P-value | ||
|---|---|---|---|---|
| Age | 1.05 | 1.03 | 1.07 | <0.0001 |
| Sex (Female vs. Male) | 1.03 | 0.59 | 1.77 | 0.92 |
| History of VTE (Yes vs. No) | 1.92 | 0.53 | 7.02 | 0.32 |
| Presence of malignancy (Yes vs. No) | 2.55 | 1.29 | 5.07 | 0.0075 |
| Presence of neurologic disease (Yes vs. No) | 0.88 | 0.5 | 1.55 | 0.65 |
| Indication for filter placement | ||||
| VTE/anticoagulation contraindication | 0.92 | 0.47 | 1.78 | 0.79 |
| VTE/anticoagulation complication | 1.69 | 0.71 | 4.02 | 0.24 |
| VTE/anticoagulation failure | 0.61 | 0.17 | 2.15 | 0.44 |
| Prophylaxis | 0.52 | 0.14 | 1.9 | 0.32 |
IVCF: Inferior vena cava filter, VTE: Venous thromboembolism, OR: Odds ratio, CI: Confidence interval
The receiver operator characteristic curve for the prediction model based on the previously published formula yielded an area under the curve of 0.66, compared to the previously published value of 0.8. The receiver operator curve illustrated in Figure 1. The sensitivity and specificity of the prediction model were estimated 64.3% and 62.0%, respectively.
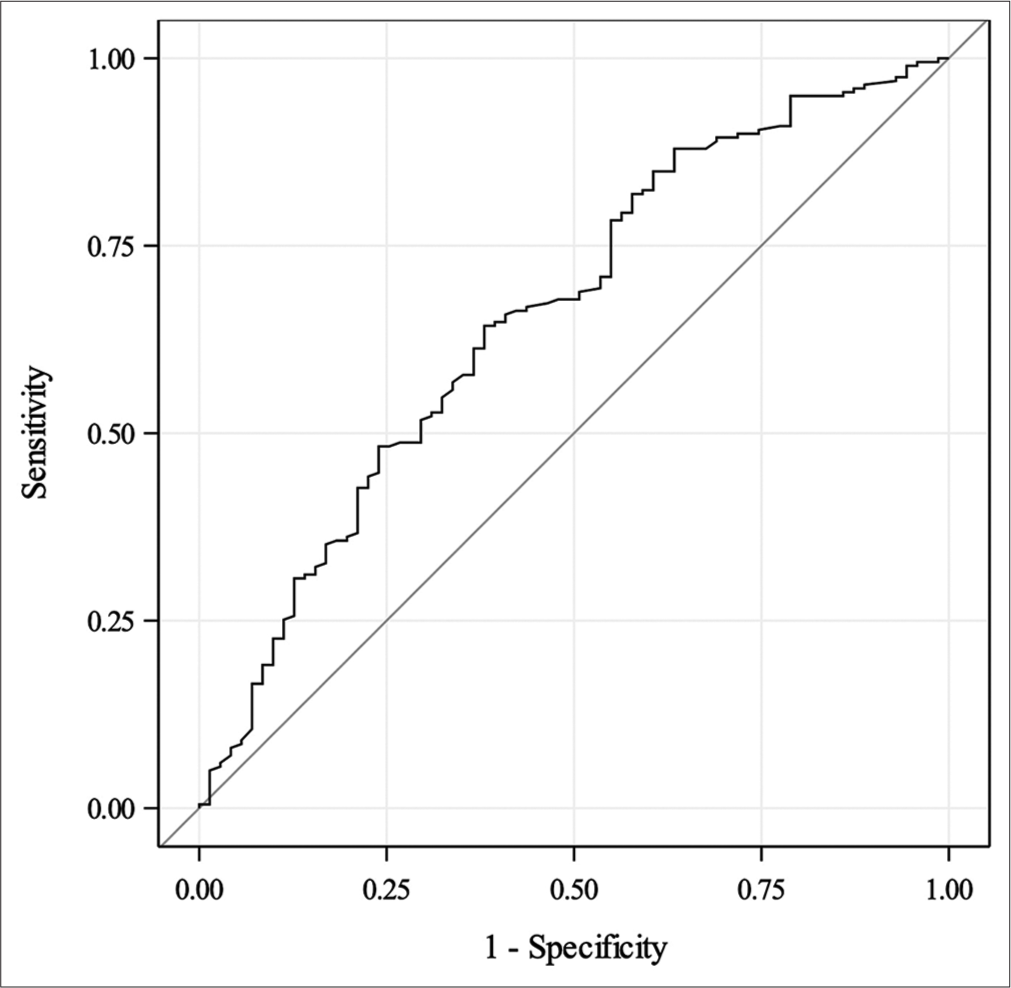
- Receiver operating characteristic curve for reference predicted probability. Area under the curve = 0.66.
DISCUSSION
Despite the availability of optional IVCFs, there are still several potential advantages of placing a permanent device. First, current evidence shows that indwelling optional filters are associated with a higher complication rate.[15-17,19] For example, in a retrospective study evaluating 449 retrievable versus 785 permanent filters, Desai et al. showed statistically significant higher overall rates of complications with retrievable filters (9% vs. 3%).[15] These included both thrombotic complications, such as lower extremity deep venous thrombosis, pulmonary embolism, and inferior vena cava thrombosis, and device-related complications, such as filter penetration, migration, or device fracture.[15] Likewise, a review of the Manufacturer and User Facility Device Experience database demonstrated that 86.8% of all reported adverse events for IVCFs were associated with optional IVCFs.[16] Second, there may be cost benefits to placing permanent devices. For instance, some authors have previously shown that the predicted cost of a permanent IVCF is lower than that of an optional device, in addition to a higher predicted rate of clinical efficacy.[17] Finally, the utilization of a permanent IVCF obviates the need for routine clinical follow-up. Without a dedicated system in place, IVCF retrieval rates are poor. However, despite an effort and success in implementation of such programs, optional filters retrieval rates are repeatedly reflected in literature to be below 60%.[10-14] One analysis of a filter retrieval program showed that despite a low percentage of patients lost to follow-up, only 28% of filters were retrieved. Almost 50% of the patients with optional filters had their filters either deemed permanent or died before a decision regarding filter retrieval.[14] These group of patients could benefit from placement of permanent IVCFs or optional IVCFs with clear intent of acting as permanent devices with no scheduled follow-up. This approach represents a more cost-effective option, emphasizing a need for improved patient selection tools.
Eifler et al. conducted a study using logistic regression analysis for quantitative prediction of optional IVCF permanence.[18] They analyzed 265 optional IVCFs placed between December 2008 and July 2011 in a retrospective manner. The authors observed patient parameters correlating with retrievability of these filters and formulated an equation that would aid clinicians in a decision between placing an optional versus a permanent filter. This equation is available as an easy-to-use online-based calculator.[20] In their multivariable model predicting filter disposition, significant factors associated with permanence were age (OR 1.03; 95% CI 1.01–1.05), male sex (OR, 3.01; 95% CI, 1.64–5.54), underlying malignancy (OR, 3.27; 95% CI, 1.77–6.03), and an indication of anticoagulation failure (OR, 8.12; 95% CI, 1.83–36.0). Significant factors associated with removal were history of VTE (OR, 0.39; 95% CI, 0.21–0.74), prophylactic filter placement indication (OR, 0.14; 95% CI, 0.04–0.43), and high-risk VTE (OR, 0.37; 95% CI, 0.15–0.94). This analysis yielded a c-statistic of the formula of 0.8, indicating a good ability to predict filter permanence.
The current data aim to externally validate this quantitative model in a different patient population. Similar to prior reports, age and presence of malignancy were significantly associated with retrievable IVCFs being kept as permanent devices. It is intuitive, that advanced age implies more comorbidities, higher chance of dying, as well as limited opportunities to follow-up for a filter retrieval in comparison with a younger patient population. Furthermore, this analysis supports the conclusions of prior studies that the presence of malignancy decreased the probability for retrieval. Sex was shown as a predictor of filter retrieval by Eifler et al.,[18] which, however, was not a statistically significant predictor in study by D’Othée et al.,[21] similarly to our study. Indications for filter placement in our patient population were not statistically significant for filter retrieval prediction. Patients with an indication for placement of anticoagulation failure, which was predictive of filter permanence in the Eifler et al.[18] cohort, were presented in very small numbers in both the reference study and the present study, which could explain discordance in the significance of this finding. Only one high-risk VTE patient was present in our cohort and was, therefore, excluded from this analysis. The number of IVCFs placed for prophylaxis at our institution was markedly lower in comparison to the study by Eifler et al,[18] which might explain the discordance between the current data and reference report. The differences in patient numbers between the two data sets are likely due to evolving standards with regard to prophylactic filter placement. The receiver operator characteristic curve based on the prediction model by Eifler et al.[18] yielded the area under the curve of 0.66 for this external patient population, compared to the previously published value of 0.8. The sensitivity and specificity of the prediction model were 64.3% and 62.0%, respectively. These findings indicate poor performance of the formula in this external patient population.
The study is limited by several factors. First, it is retrospective in nature, which limits data collection to that which is available. Second, there is no standardized process at the authors’ institution for the selection of a permanent or optional IVCF. This means that patient selection was subject to operator preferences and bias as well as filter availability at the time of placement. Third, the decision to attempt filter retrieval is subject to physician bias and patients’ preferences. In the authors’ anecdotal experience, patients’ preferences have a significant role in the decision to attempt retrieval. Fourth, the two studies were performed at different time points. Even though the purpose of the paper was to externally validate the previously published quantitative model, evolving guidelines regarding filter placement may have had a role in discrepancies between the two populations. Regardless of these limitations, this analysis shows that the application of this quantitative model to a different patient population resulted in a relatively poor predictive performance. Nevertheless, placement of permanent IVCFs in patients with advanced age and presence of malignancy should be considered, as these factors were repeatedly associated with lower likelihood of retrieval in va rious patient populations. Larger scale studies to derive a better model for selection of candidates for permanent filter placement should be considered.
CONCLUSION
Advanced age and presence of malignancy are associated with optional IVCFs being kept as permanent devices. However, the previously published formula did not yield an accurate quantitative prediction in this external patient population.
Ethical approval
The research/study was approved by the Institutional Review Board at University of Alabama at Birmingham, number IRB-300000557, dated December 09, 2018.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Society of Interventional Radiology clinical practice guideline for inferior vena cava filters in the treatment of patients with venous thromboembolic disease: Developed in collaboration with the American College of Cardiology, American College of Chest Physicians, American College of Surgeons Committee on Trauma, American Heart Association, Society for Vascular Surgery, and Society for Vascular Medicine. J Vasc Interv Radiol. 2020;31:1529-44.
- [CrossRef] [Google Scholar]
- Practice management guidelines for the prevention of venous thromboembolism in trauma patients: The EAST practice management guidelines work group. J Trauma. 2002;53:142-64.
- [CrossRef] [Google Scholar]
- Quality improvement guidelines for the performance of inferior vena cava filter placement for the prevention of pulmonary embolism. J Vasc Interv Radiol. 2011;22:1499-506.
- [CrossRef] [Google Scholar]
- ACR Appropriateness Criteria® Radiologic management of venous thromboembolism-inferior vena cava filters. J Am Coll Radiol. 2019;16:S214-26.
- [CrossRef] [Google Scholar]
- Antithrombotic therapy for VTE disease: Antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 Suppl):e419S-96.
- [Google Scholar]
- 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European respiratory society (ERS) Eur Heart J. 2020;41:543-603.
- [CrossRef] [Google Scholar]
- National trends in utilization of inferior vena cava filters in the United States, 2000-2009. J Vasc Surg Venous Lymphat Disord. 2014;2:15-20.
- [CrossRef] [Google Scholar]
- Removing retrievable inferior vena cava filters. 2010. Initial communication. Available from: https://wayback.archive-it.org/7993/20161022180008 http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm221676.htm [Last accessed on 2024 Aug 01]
- [Google Scholar]
- Removing retrievable inferior vena cava filters. 2014. FDA safety communication. Available from: https://wayback.archive-it.org/7993/20161022044053 http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm396377.htm [Last accessed on 2024 Aug 01]
- [Google Scholar]
- Improving inferior vena cava filter retrieval rates: Impact of a dedicated inferior vena cava filter clinic. J Vasc Interv Radiol. 2010;21:1847-51.
- [CrossRef] [Google Scholar]
- Improved removal rates for retrievable inferior vena cava filters with the use of a “filter registry”. Am Surg. 2012;78:94-7.
- [CrossRef] [Google Scholar]
- Institutional protocol improves retrievable inferior vena cava filter recovery rate. Surgery. 2009;146:809-16.
- [CrossRef] [Google Scholar]
- Implementation of an institutional protocol to improve inferior vena cava utilization and outcomes. J Thromb Thrombolysis. 2017;44:190-6.
- [CrossRef] [Google Scholar]
- Effect of a dedicated inferior vena cava filter retrieval program on retrieval rates and number of patients lost to follow-up. Diagn Interv Radiol. 2020;26:40-4.
- [CrossRef] [Google Scholar]
- Complications of indwelling retrievable versus permanent inferior vena cava filters. J Vasc Surg Venous Lymphat Disord. 2014;2:166-73.
- [CrossRef] [Google Scholar]
- Comparison of complication rates associated with permanent and retrievable inferior vena cava filters: A review of the MAUDE database. J Vasc Interv Radiol. 2014;25:1181-5.
- [CrossRef] [Google Scholar]
- Permanent inferior vena cava filters offer greater expected patient utility at lower predicted cost. J Vasc Surg Venous Lymphat Disord. 2020;8:583-92.e5.
- [CrossRef] [Google Scholar]
- Optional or permanent: Clinical factors that optimize inferior vena cava filter utilization. J Vasc Interv Radiol. 2013;24:35-40.
- [CrossRef] [Google Scholar]
- A comparison of clinical outcomes with retrievable and permanent inferior vena cava filters. J Vasc Interv Radiol. 2008;19:393-9.
- [CrossRef] [Google Scholar]
- Likelihood of retrieval calculator. Available from: https://ivcfilter.nm.org/calculator-original.html [Last accessed on 2024 Aug 01]
- [Google Scholar]
- Retrievable versus permanent caval filter procedures: When are they cost-effective for interventional radiology? J Vasc Interv Radiol. 2008;19:384-92.
- [CrossRef] [Google Scholar]








